Back End Revenue Cycle Management Market Report
Published Date: 31 January 2026 | Report Code: back-end-revenue-cycle-management
Back End Revenue Cycle Management Market Size, Share, Industry Trends and Forecast to 2033
This comprehensive market report for Back End Revenue Cycle Management provides insights into market size, segmentation, trends, and forecasts from 2023 to 2033. It analyzes key regional markets and industry leaders, offering valuable data for stakeholders and investors.
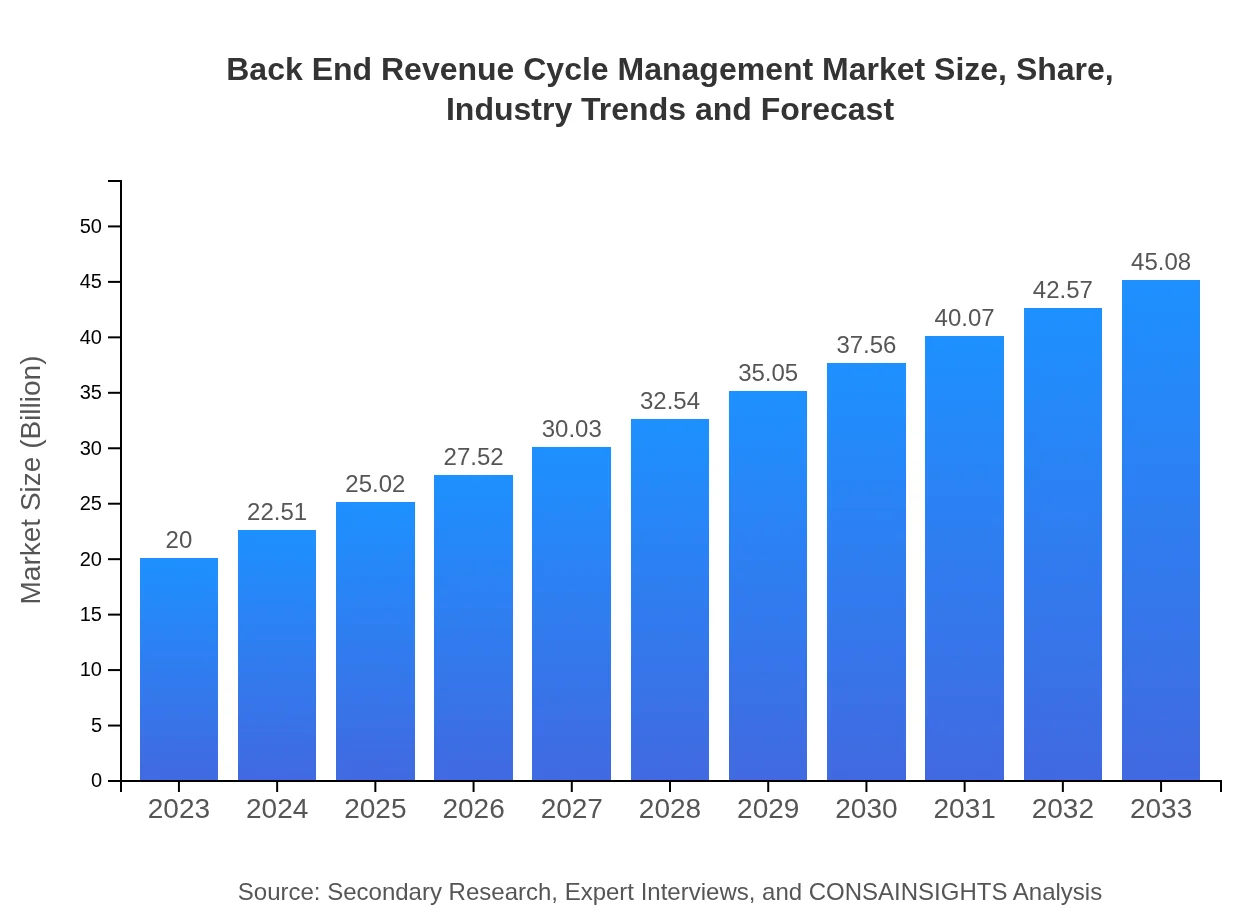
| Metric | Value |
|---|---|
| Study Period | 2023 - 2033 |
| 2023 Market Size | $20.00 Billion |
| CAGR (2023-2033) | 8.2% |
| 2033 Market Size | $45.08 Billion |
| Top Companies | Optum, Cerner Corporation, Change Healthcare, McKesson Corporation |
| Last Modified Date | 31 January 2026 |
Back End Revenue Cycle Management Market Overview
Customize Back End Revenue Cycle Management Market Report market research report
- ✔ Get in-depth analysis of Back End Revenue Cycle Management market size, growth, and forecasts.
- ✔ Understand Back End Revenue Cycle Management's regional dynamics and industry-specific trends.
- ✔ Identify potential applications, end-user demand, and growth segments in Back End Revenue Cycle Management
What is the Market Size & CAGR of Back End Revenue Cycle Management market in 2023 and 2033?
Back End Revenue Cycle Management Industry Analysis
Back End Revenue Cycle Management Market Segmentation and Scope
Tell us your focus area and get a customized research report.
Back End Revenue Cycle Management Market Analysis Report by Region
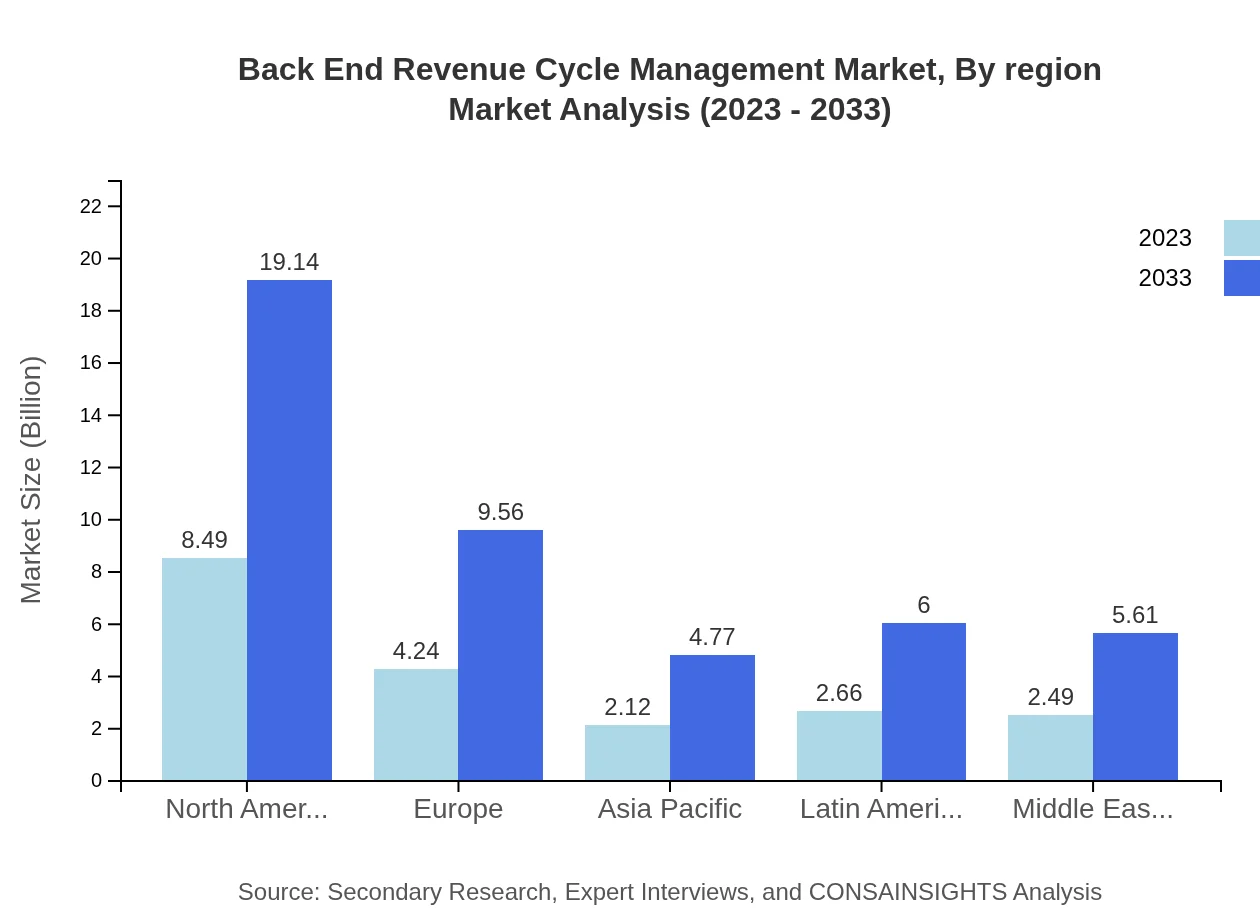
Europe Back End Revenue Cycle Management Market Report:
The European market for Back End RCM stood at $5.27 billion in 2023 and is projected to expand to $11.88 billion by 2033. Factors such as a focus on improving patient care and addressing rising operational costs are pivotal in this region's growth.Asia Pacific Back End Revenue Cycle Management Market Report:
In Asia Pacific, the market was valued at $4.15 billion in 2023 and is expected to grow to $9.36 billion by 2033. This growth is fueled by increasing healthcare expenditure, digital transformation in health services, and the rising demand for efficient billing and collection processes in countries like India and China.North America Back End Revenue Cycle Management Market Report:
North America holds a significant share of the market, estimated at $7.17 billion in 2023, anticipated to grow to $16.16 billion by 2033. This region's growth is driven by the presence of major market players, continuous technological advancements, and regulatory enforcement towards efficient billing practices.South America Back End Revenue Cycle Management Market Report:
In South America, the Back End RCM market reported a size of $1.52 billion in 2023, projected to rise to $3.43 billion by 2033. Key factors for this growth include the adoption of electronic health records and improvements in healthcare infrastructure in countries such as Brazil and Argentina.Middle East & Africa Back End Revenue Cycle Management Market Report:
The Back End RCM market in the Middle East and Africa was valued at $1.88 billion in 2023, with expectations to reach $4.25 billion by 2033. Growth in this region is encouraged by investments in health technology, increasing health insurance penetration, and the need for improved revenue management.Tell us your focus area and get a customized research report.
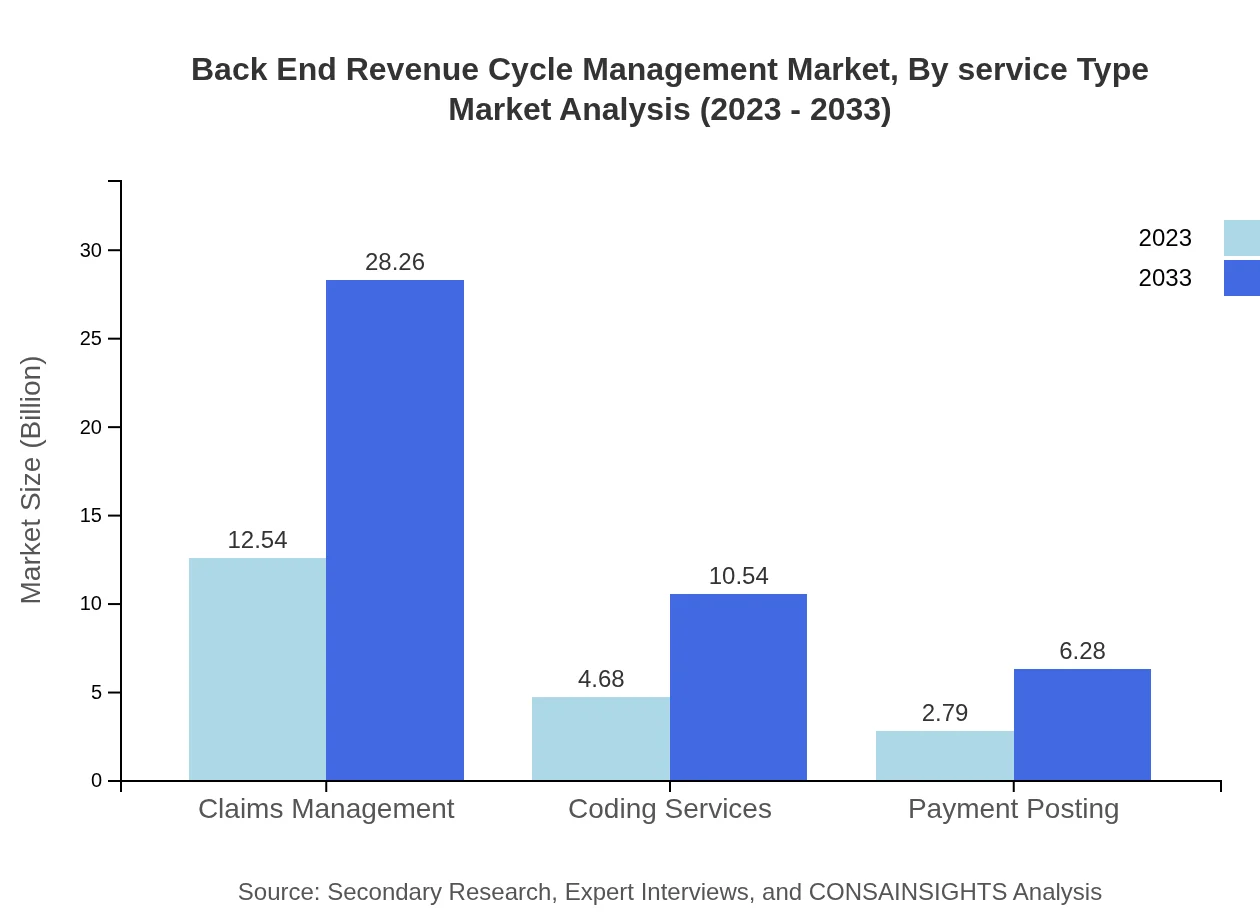
Back End Revenue Cycle Management Market Analysis By Service Type
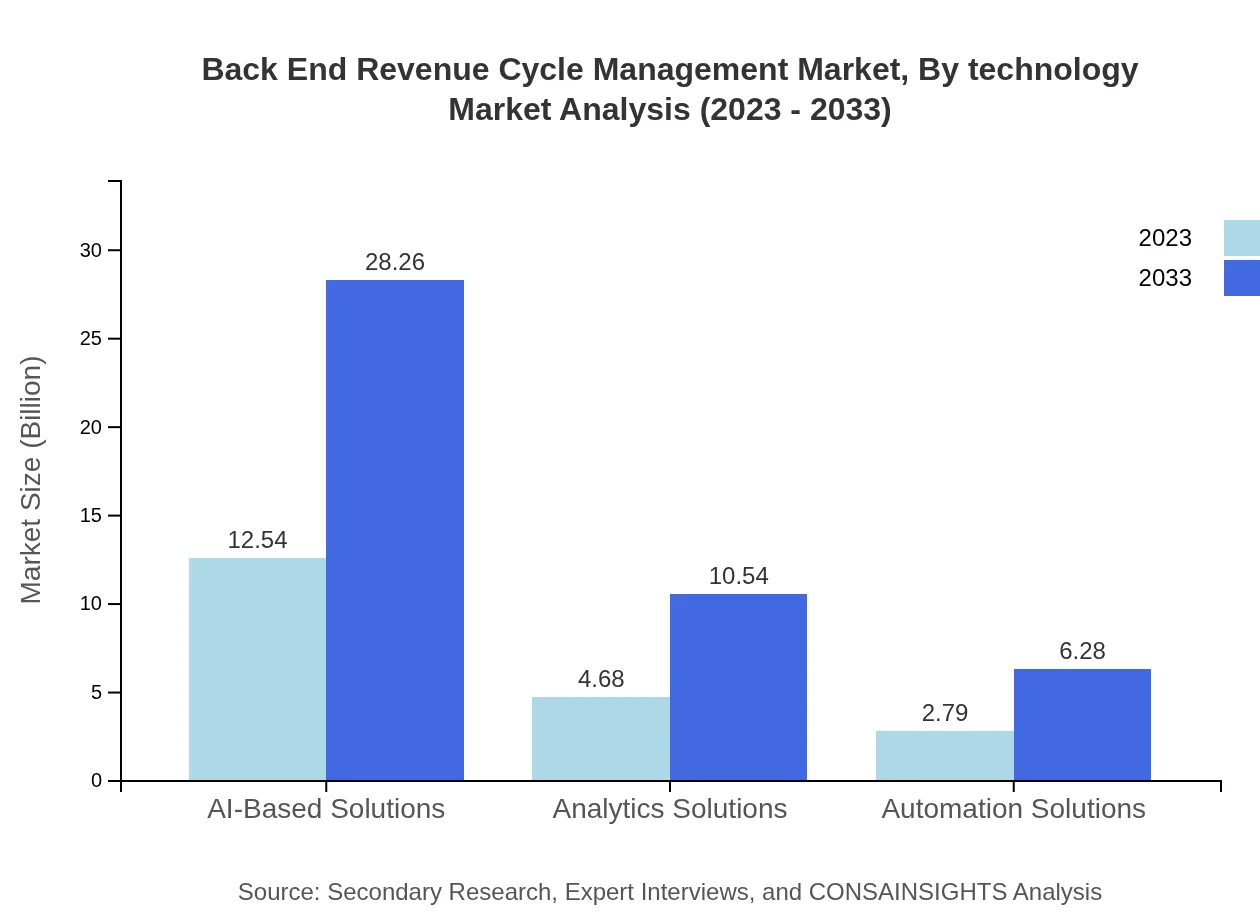
The service type segmentation reveals that Claims Management leads the market with significant revenue, expected to reach $28.26 billion by 2033 from $12.54 billion in 2023. Other notable segments include Coding Services and Payment Posting, both experiencing steady growth as healthcare professionals seek efficiency in reimbursement processes.
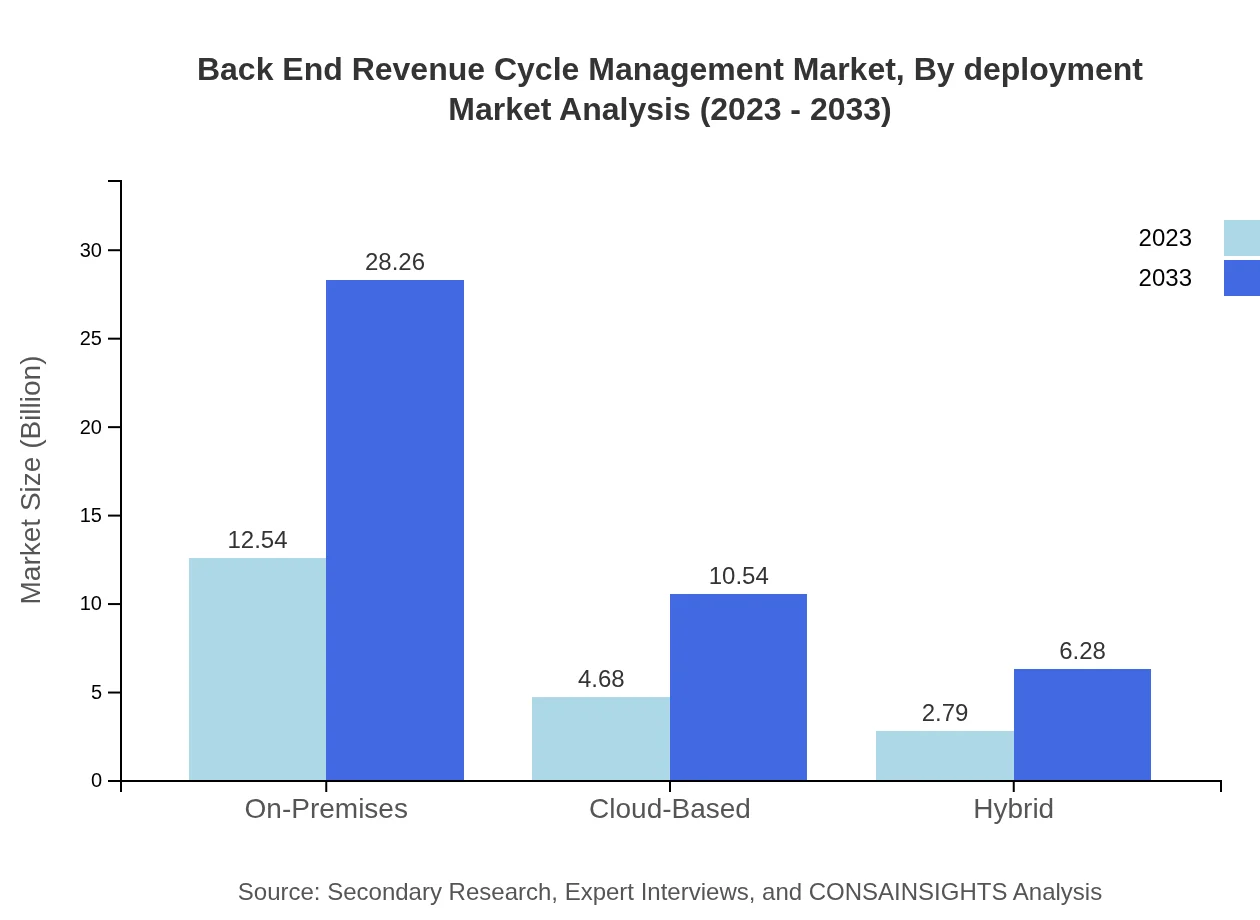
Back End Revenue Cycle Management Market Analysis By Deployment
By deployment type, On-Premises solutions dominate the Back End RCM market due to customization flexibility and data security concerns. However, Cloud-Based deployments are rapidly gaining popularity, expected to grow significantly over the next decade as providers seek scalable and cost-effective solutions.
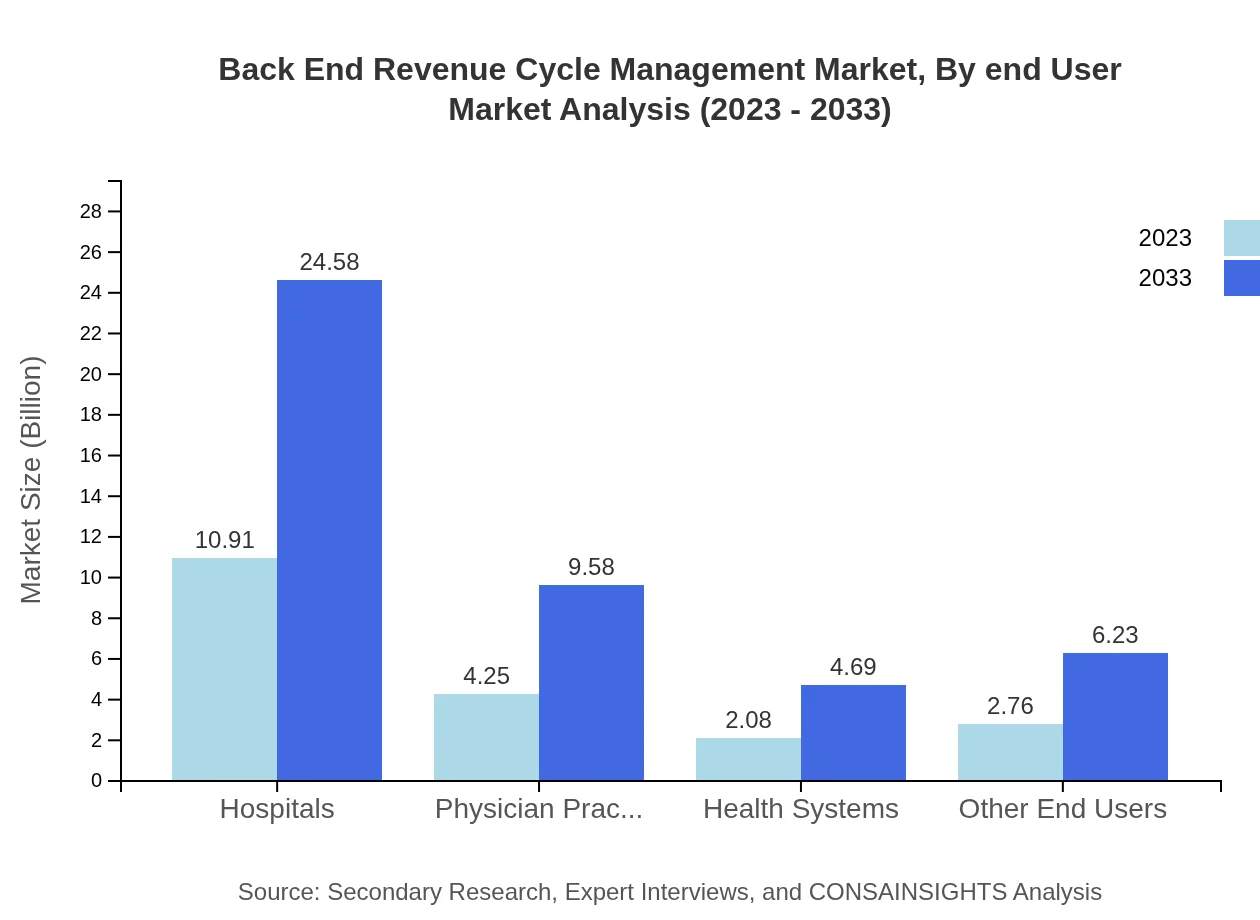
Back End Revenue Cycle Management Market Analysis By End User
Within the end-user segment, Hospitals represent the largest market share, significantly driving revenue growth. The increasing focus on operational efficiency and cost control in hospitals mandates the use of advanced RCM solutions.
Back End Revenue Cycle Management Market Analysis By Technology
The Back End RCM market is rapidly integrating advanced technologies such as AI and machine learning, enhancing predictive analytics capabilities and process automation. These technologies substantially improve the accuracy of billing and expedite claims processing.
Back End Revenue Cycle Management Market Analysis By Region
Regionally, North America continues to lead in market share, followed by Europe and Asia Pacific. Each region exhibits distinct growth drivers, from regulatory requirements in North America to the burgeoning healthcare markets in Asia Pacific.
Back End Revenue Cycle Management Market Trends and Future Forecast
Tell us your focus area and get a customized research report.
Global Market Leaders and Top Companies in Back End Revenue Cycle Management Industry
Optum:
Optum offers health services and information technology solutions, providing comprehensive RCM services that optimize revenue and reduce operational costs for healthcare providers.Cerner Corporation:
Cerner is known for its health information technology designed to enhance RCM processes, assisting hospitals and physician practices in revenue optimization.Change Healthcare:
Change Healthcare specializes in healthcare technology solutions, focusing on improving patient outcomes through smarter payment and billing processes backed by advanced analytics.McKesson Corporation:
McKesson provides a broad range of RCM services, supporting healthcare organizations in managing their billing, collections, and financial reporting more effectively.We're grateful to work with incredible clients.









FAQs
What is the market size of Back-End Revenue Cycle Management?
The Back-End Revenue Cycle Management market is projected to reach approximately $20 billion by 2033, growing at a CAGR of 8.2%. This growth reflects increasing demand for effective financial management solutions within healthcare.
What are the key market players or companies in the Back-End Revenue Cycle Management industry?
Key players in the Back-End Revenue Cycle Management industry include major healthcare technology companies and service providers focusing on innovative financial solutions, enhancing operational efficiency and revenue integrity across healthcare institutions.
What are the primary factors driving the growth in the Back-End Revenue Cycle Management industry?
Growth drivers include an increasing emphasis on revenue integrity, regulatory compliance pressures, advancements in technology, the need for operational efficiency, and a shift towards value-based care models in the healthcare sector.
Which region is the fastest Growing in Back-End Revenue Cycle Management?
North America is the fastest-growing region, with the market size projected to expand from $7.17 billion in 2023 to $16.16 billion by 2033, reflecting strong demand and technology adoption in the healthcare sector.
Does ConsaInsights provide customized market report data for the Back-End Revenue Cycle Management industry?
Yes, ConsaInsights offers customized market report data tailored to specific needs in the Back-End Revenue Cycle Management industry, allowing clients to delve into particular segments or trends of interest.
What deliverables can I expect from this Back-End Revenue Cycle Management market research project?
Deliverables include comprehensive market analysis reports, segmentation insights, competitive landscape assessments, regional forecasts, and actionable recommendations tailored to your business needs.
What are the market trends of Back-End Revenue Cycle Management?
Current trends include increased automation, the adoption of AI-based solutions, a shift towards cloud-based technologies, enhanced data analytics use, and growing focus on improving patient billing experiences.