Care Management Solutions Market Report
Published Date: 31 January 2026 | Report Code: care-management-solutions
Care Management Solutions Market Size, Share, Industry Trends and Forecast to 2033
This market report provides an in-depth analysis of the Care Management Solutions industry, highlighting key trends, market size, and competitive landscape. Insights and projections extend from 2023 to 2033 to aid stakeholders in strategic decision-making.
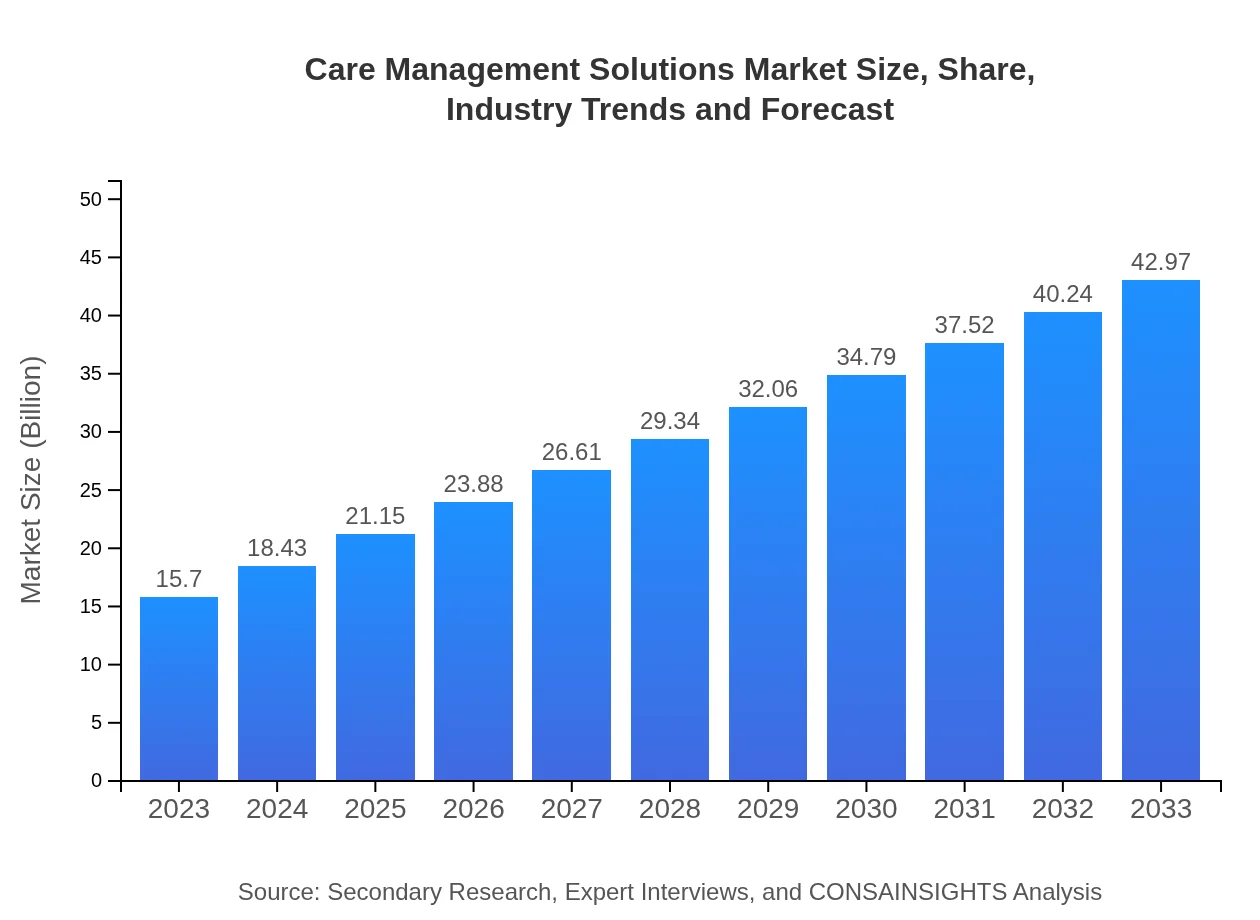
| Metric | Value |
|---|---|
| Study Period | 2023 - 2033 |
| 2023 Market Size | $15.70 Billion |
| CAGR (2023-2033) | 10.2% |
| 2033 Market Size | $42.97 Billion |
| Top Companies | Epic Systems Corporation, Cerner Corporation, IBM Watson Health, McKesson Corporation |
| Last Modified Date | 31 January 2026 |
Care Management Solutions Market Overview
Customize Care Management Solutions Market Report market research report
- ✔ Get in-depth analysis of Care Management Solutions market size, growth, and forecasts.
- ✔ Understand Care Management Solutions's regional dynamics and industry-specific trends.
- ✔ Identify potential applications, end-user demand, and growth segments in Care Management Solutions
What is the Market Size & CAGR of Care Management Solutions market in 2023?
Care Management Solutions Industry Analysis
Care Management Solutions Market Segmentation and Scope
Tell us your focus area and get a customized research report.
Care Management Solutions Market Analysis Report by Region
Europe Care Management Solutions Market Report:
Europe's market is anticipated to climb from $3.96 billion in 2023 to $10.83 billion by 2033. Rising chronic disease rates and a focus on personalized healthcare solutions are influencing this growth, along with regulatory support for integrated care models.Asia Pacific Care Management Solutions Market Report:
The Asia-Pacific market is expected to grow from $3.33 billion in 2023 to $9.11 billion by 2033. Factors driving this growth include an expanding elderly population and greater emphasis on preventive care and chronic disease management. Governments are also investing heavily in digital healthcare solutions to improve service delivery.North America Care Management Solutions Market Report:
Dominating the global Care Management Solutions market, North America is set to expand from $5.98 billion in 2023 to $16.38 billion by 2033. The region benefits from advanced healthcare infrastructure, strong demand for tech-driven patient management systems, and active investment in healthcare IT.South America Care Management Solutions Market Report:
In South America, the market is projected to increase from $1.44 billion in 2023 to $3.93 billion by 2033. The growth is fueled by increasing healthcare funding and the push towards integrated care systems, aided by innovative start-ups introducing mobile and cloud-based solutions.Middle East & Africa Care Management Solutions Market Report:
The Middle East and Africa market is expected to grow from $0.99 billion in 2023 to $2.72 billion by 2033. Increasing investment in healthcare infrastructure, coupled with rising awareness of chronic diseases, supports the demand for effective care management solutions.Tell us your focus area and get a customized research report.
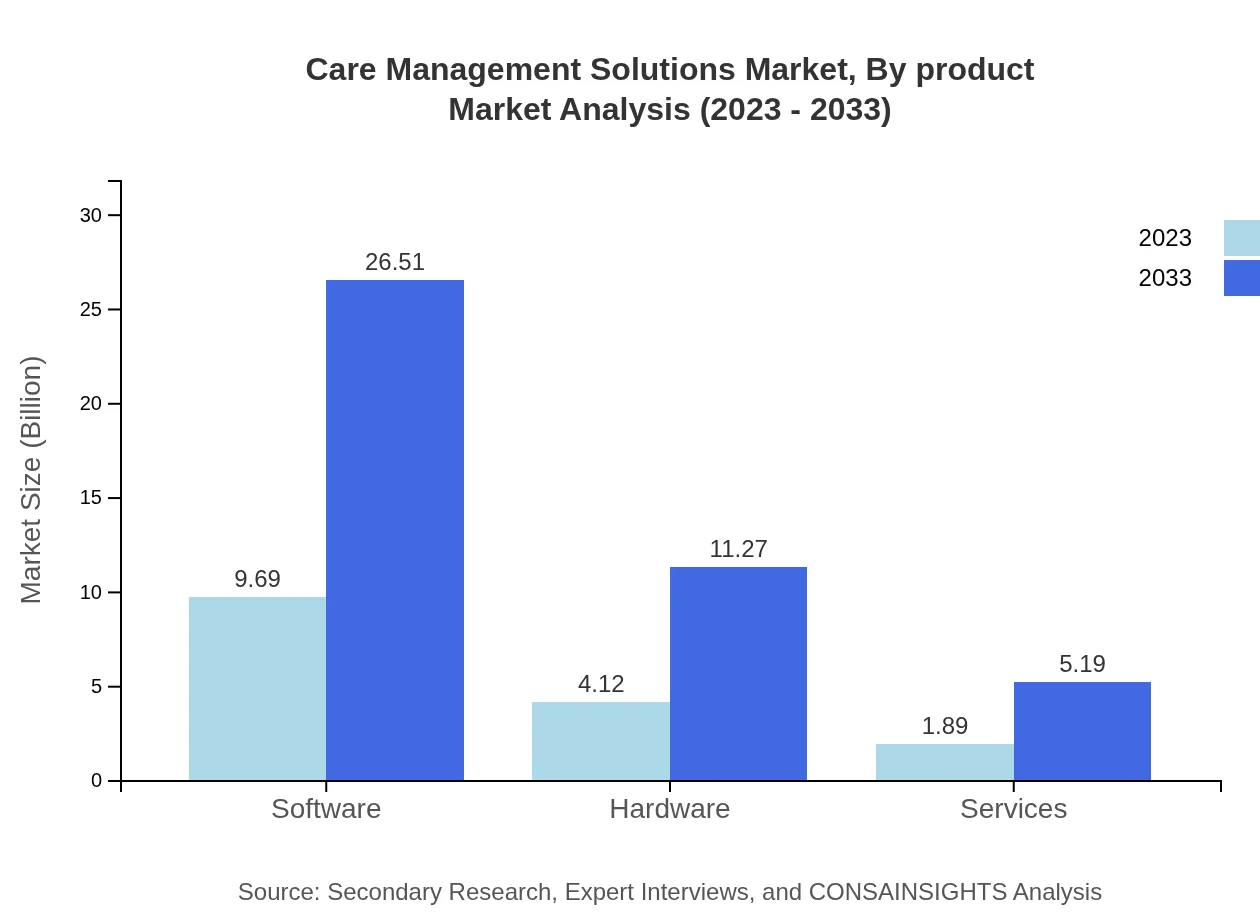
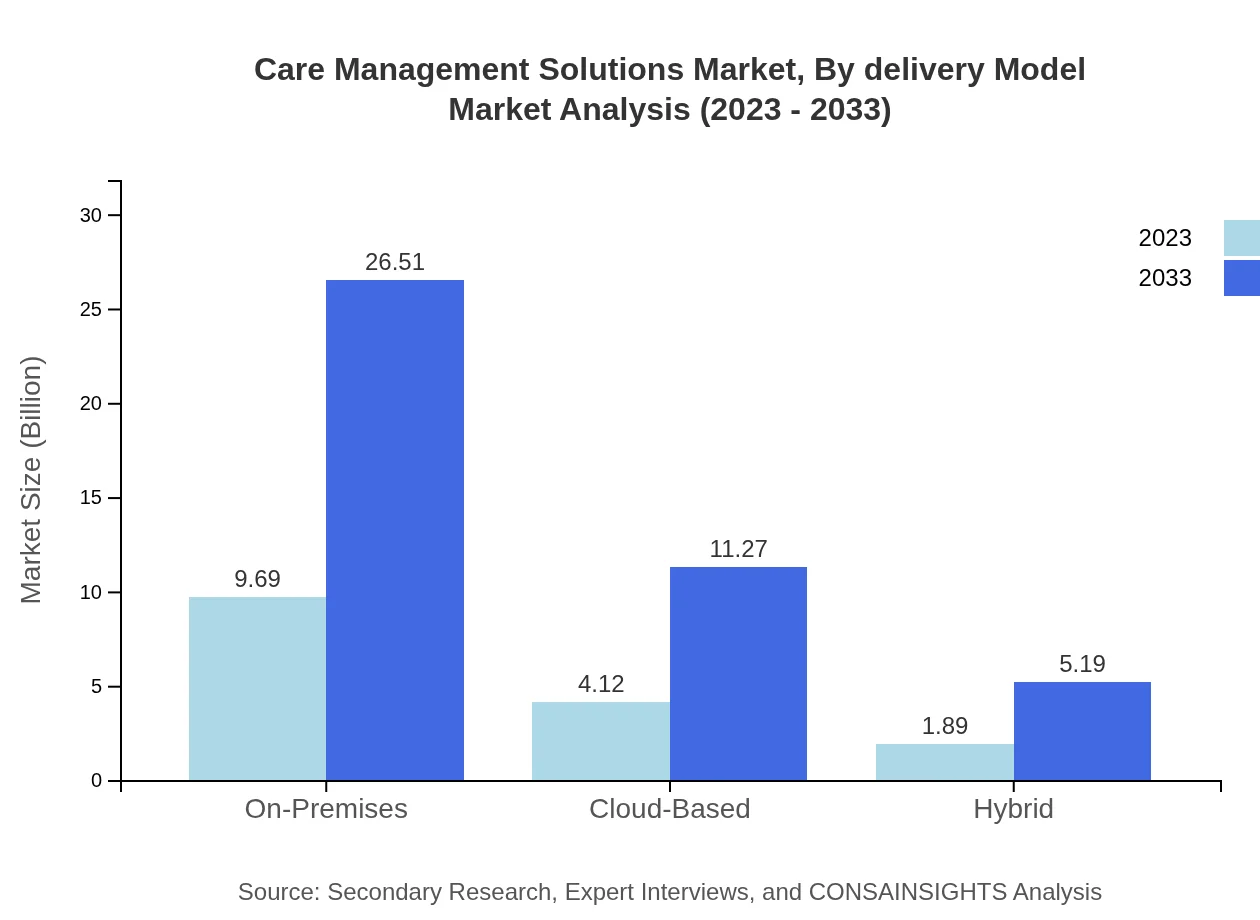
Care Management Solutions Market Analysis By Product
In the product segment, the software category leads with a market size of $9.69 billion in 2023, expected to rise to $26.51 billion by 2033, holding a market share of 61.7%. Hardware and services are also significant, contributing $4.12 billion and $1.89 billion respectively in 2023, with forecasts anticipating growth to $11.27 billion and $5.19 billion by 2033.
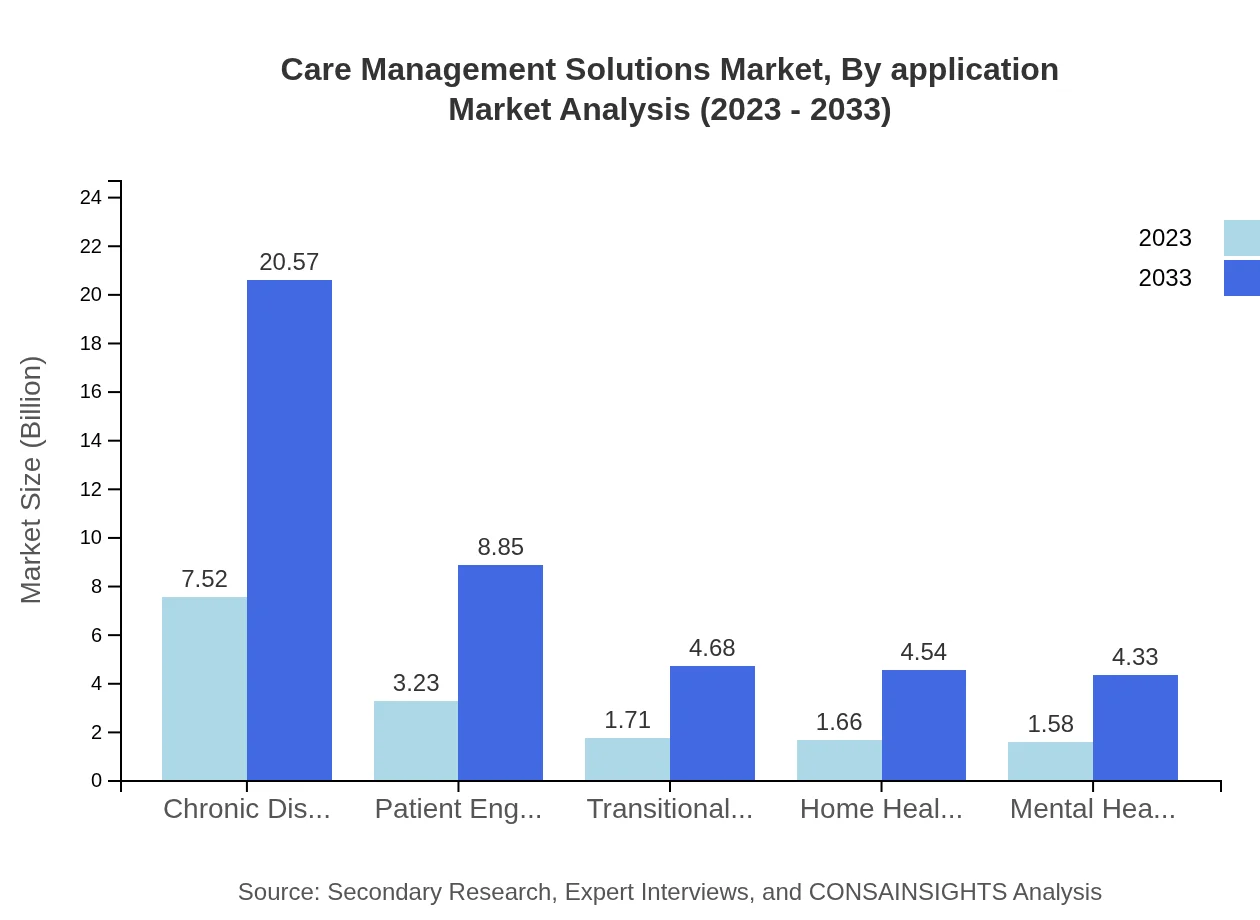
Care Management Solutions Market Analysis By Application
Key applications include chronic disease management, mental health management, and patient engagement, with chronic disease management being vital at $7.52 billion in 2023, projected to grow to $20.57 billion by 2033, reflecting a 47.88% market share.
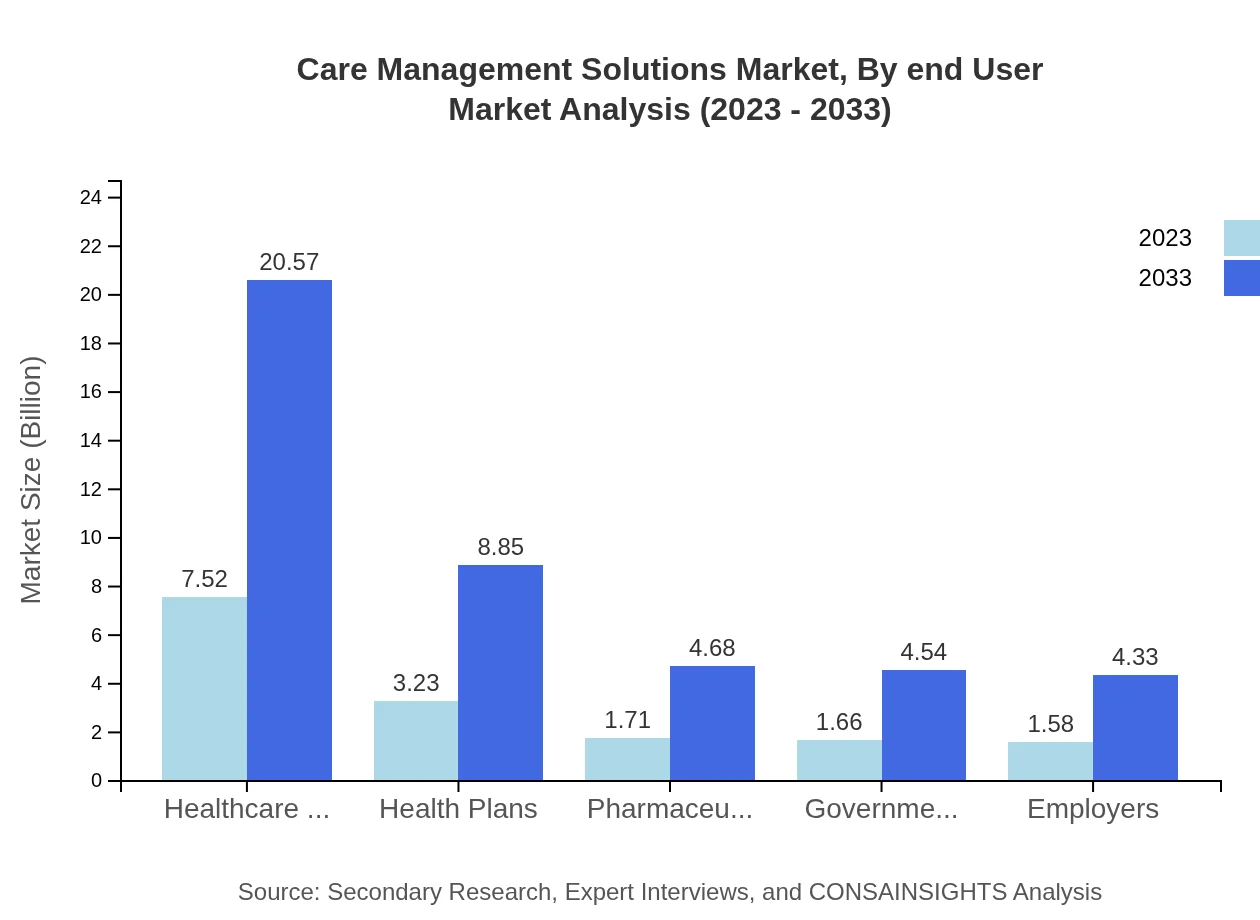
Care Management Solutions Market Analysis By End User
The end-user segment analysis highlights healthcare providers as the dominant group, valued at $7.52 billion in 2023, anticipated to grow to $20.57 billion by 2033, while health plans, government organizations, and employers also represent sizeable markets due to increasing regulatory requirements and demand for care efficiency.
Care Management Solutions Market Analysis By Delivery Model
On-premises solutions are prominent, leading with a market size of $9.69 billion in 2023. However, cloud-based solutions are gaining traction, projected to grow from $4.12 billion to $11.27 billion by 2033, driven by the demand for scalability and flexibility in healthcare solutions.
Care Management Solutions Market Analysis By Region Focus
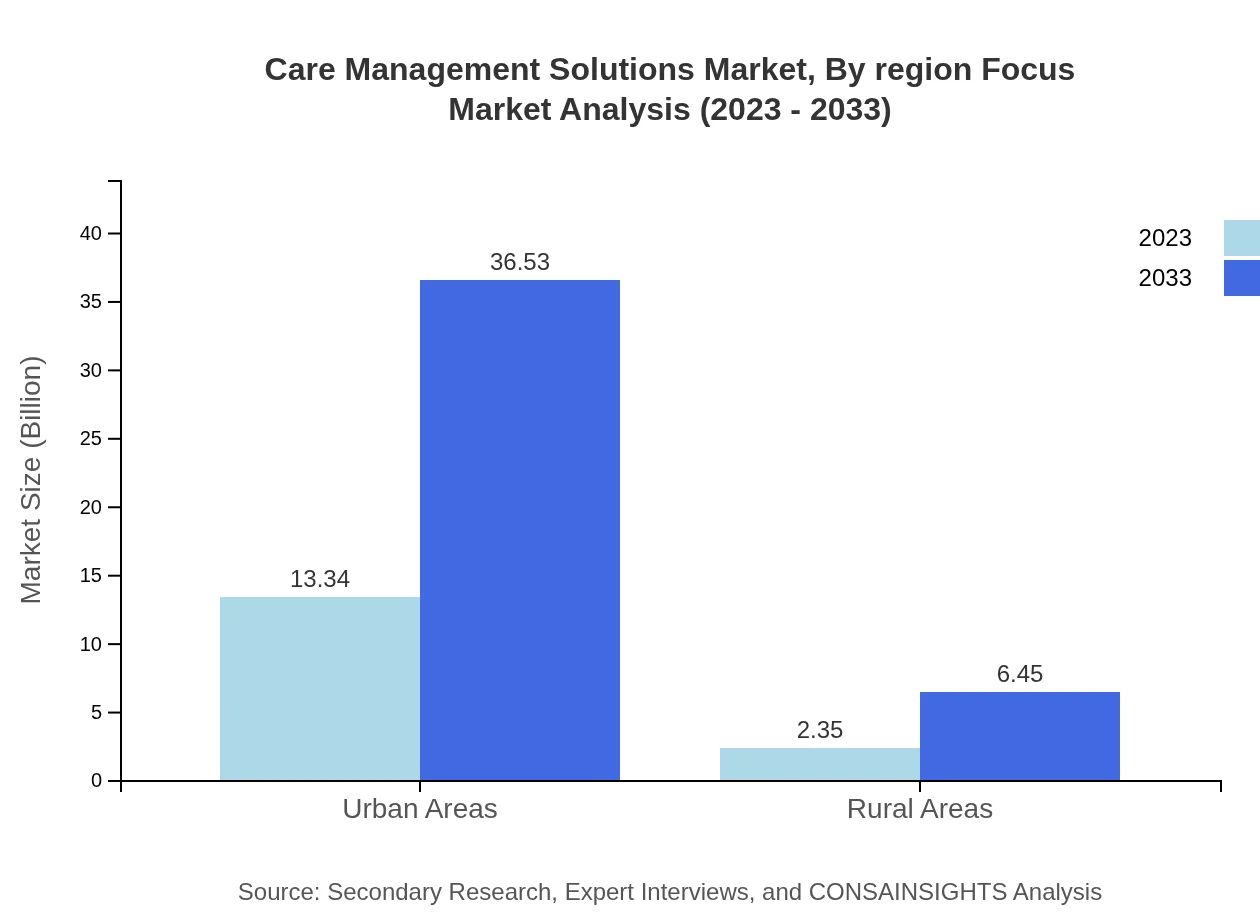
Regional focuses reveal that urban areas contribute significantly to market revenues, with a size of $13.34 billion in 2023, while rural areas, although smaller at $2.35 billion, indicate potential for growth through targeted care management initiatives.
Care Management Solutions Market Trends and Future Forecast
Tell us your focus area and get a customized research report.
Global Market Leaders and Top Companies in Care Management Solutions Industry
Epic Systems Corporation:
A leader in healthcare software solutions, Epic provides comprehensive electronic health records and care management systems, enhancing patient outcomes through better data utilization.Cerner Corporation:
Known for its innovative health information technology solutions, Cerner specializes in integrated care management systems that support patient engagement and chronic disease management.IBM Watson Health:
Utilizing AI technology, IBM Watson Health delivers data-driven insights to healthcare providers, promoting personalized treatment plans and efficient care delivery.McKesson Corporation:
A prominent pharmaceutical distribution services company, McKesson also provides innovative healthcare technology solutions that assist in care management and prescription services.We're grateful to work with incredible clients.









FAQs
What is the market size of care Management Solutions?
The global Care Management Solutions market is projected to reach approximately $15.7 billion by 2033, growing from $15.7 billion in 2023. It is expected to expand at a compound annual growth rate (CAGR) of 10.2% through the forecast period.
What are the key market players or companies in this care management solutions industry?
Key players in the Care Management Solutions industry include Microsoft, IBM, Cerner Corporation, Allscripts Healthcare Solutions, and Optum. Their competitive presence is vital in shaping the technological advancements and offerings within the market.
What are the primary factors driving the growth in the care management solutions industry?
Growth in the care management solutions industry is driven by increasing demand for improved patient outcomes, rising chronic diseases, technological advancements, and government initiatives aimed at enhancing healthcare delivery and management systems across various platforms.
Which region is the fastest Growing in the care management solutions?
North America is the fastest-growing region, expected to rise from $5.98 billion in 2023 to $16.38 billion by 2033. Asia Pacific follows, with growth from $3.33 billion to $9.11 billion within the same timeframe.
Does ConsaInsights provide customized market report data for the care management solutions industry?
Yes, ConsaInsights offers customized market report data tailored to specific needs within the care management solutions industry, allowing clients to gauge market dynamics, analyze trends, and identify critical factors relevant to their business.
What deliverables can I expect from this care management solutions market research project?
Deliverables for the care management solutions market research project include comprehensive market analysis reports, regional data insights, competitive landscape summaries, growth forecasts, and detailed segment analyses to assist stakeholders in strategic decision-making.
What are the market trends of care management solutions?
Key market trends in care management solutions include increasing adoption of cloud-based services, higher integration of AI and machine learning, a focus on patient engagement strategies, and the rise of advanced analytics to improve healthcare outcomes.