Healthcare Fraud Analytics Market Report
Published Date: 31 January 2026 | Report Code: healthcare-fraud-analytics
Healthcare Fraud Analytics Market Size, Share, Industry Trends and Forecast to 2033
This report comprehensively analyzes the Healthcare Fraud Analytics market, examining market size, trends, segmentation, and forecasts from 2023 to 2033, providing valuable insights for stakeholders and decision-makers in the healthcare sector.
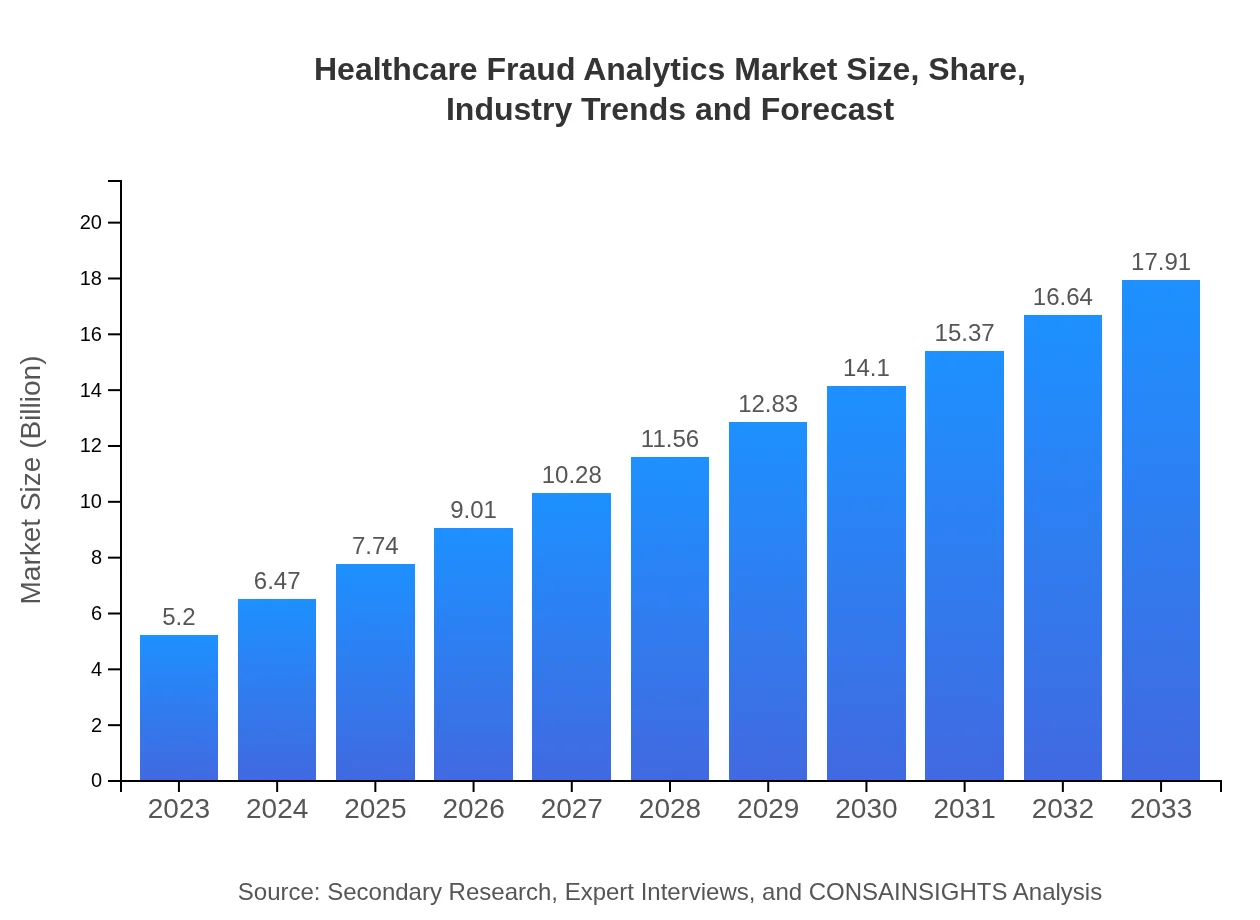
| Metric | Value |
|---|---|
| Study Period | 2023 - 2033 |
| 2023 Market Size | $5.20 Billion |
| CAGR (2023-2033) | 12.6% |
| 2033 Market Size | $17.91 Billion |
| Top Companies | IBM Corporation, Optum Inc., Cognizant Technology Solutions, SAS Institute Inc., HCL Technologies |
| Last Modified Date | 31 January 2026 |
Healthcare Fraud Analytics Market Overview
Customize Healthcare Fraud Analytics Market Report market research report
- ✔ Get in-depth analysis of Healthcare Fraud Analytics market size, growth, and forecasts.
- ✔ Understand Healthcare Fraud Analytics's regional dynamics and industry-specific trends.
- ✔ Identify potential applications, end-user demand, and growth segments in Healthcare Fraud Analytics
What is the Market Size & CAGR of Healthcare Fraud Analytics market in 2023?
Healthcare Fraud Analytics Industry Analysis
Healthcare Fraud Analytics Market Segmentation and Scope
Tell us your focus area and get a customized research report.
Healthcare Fraud Analytics Market Analysis Report by Region
Europe Healthcare Fraud Analytics Market Report:
The European market is also significant, with a forecasted growth from USD 1.56 billion in 2023 to USD 5.39 billion by 2033. Increased awareness of healthcare fraud and stringent regulations across EU nations are primary growth factors influencing this market.Asia Pacific Healthcare Fraud Analytics Market Report:
In the Asia Pacific region, the Healthcare Fraud Analytics market is expected to grow from USD 0.97 billion in 2023 to USD 3.33 billion by 2033. This growth is driven by the adoption of digital healthcare solutions and the increasing focus on healthcare fraud prevention in emerging markets like India and China, where healthcare spending is rising rapidly.North America Healthcare Fraud Analytics Market Report:
North America is currently the leading region in the Healthcare Fraud Analytics market, projected to increase from USD 1.94 billion in 2023 to USD 6.69 billion by 2033. The region's strong regulatory framework and high healthcare expenditure significantly drive the demand for advanced analytics solutions.South America Healthcare Fraud Analytics Market Report:
The South American market shows a modest growth trajectory with estimated market size growing from USD 0.06 billion in 2023 to USD 0.20 billion by 2033. Economic factors and an evolving healthcare landscape contribute to this growth, albeit at a slower pace due to varying regulatory environments.Middle East & Africa Healthcare Fraud Analytics Market Report:
In the Middle East and Africa, the market is expected to grow from USD 0.67 billion in 2023 to USD 2.31 billion by 2033. The increasing digital transformation within healthcare infrastructures promotes investment in analytics to combat fraud and streamline operations.Tell us your focus area and get a customized research report.
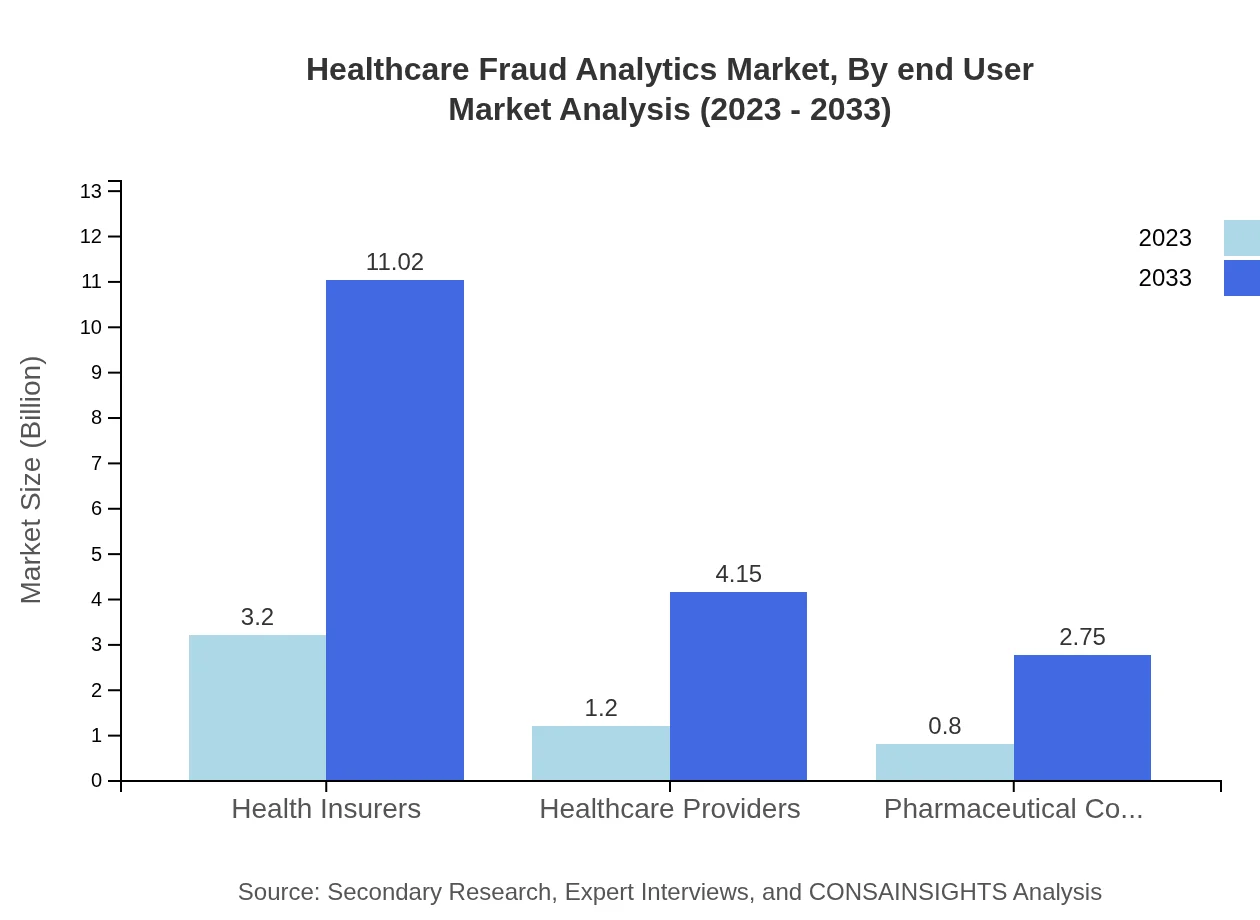
Healthcare Fraud Analytics Market Analysis By End User
Health Insurers comprise the largest end-user segment, with market values reaching USD 3.20 billion in 2023 and expected to grow to USD 11.02 billion by 2033, representing a market share of 61.52%. Healthcare Providers and Pharmaceutical Companies are also significant, with respective sizes of USD 1.20 billion (23.15% share) and USD 0.80 billion (15.33% share) in 2023. These segments play crucial roles in deploying analytics to detect and prevent fraud.
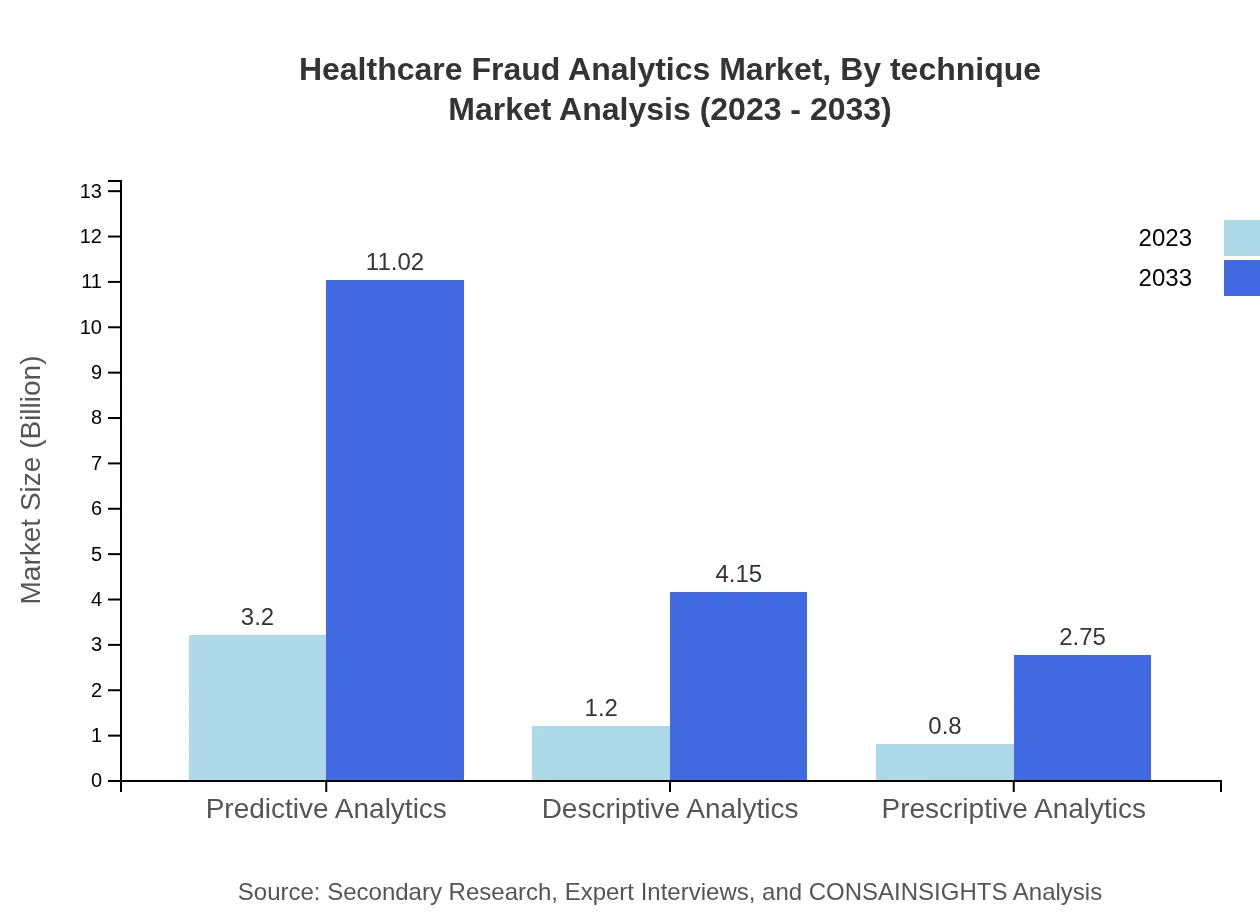
Healthcare Fraud Analytics Market Analysis By Technique
Predictive Analytics leads the segment with market sizes of USD 3.20 billion in 2023, rising to USD 11.02 billion by 2033, with a share of 61.52%. Descriptive Analytics and Prescriptive Analytics follow, each showing growth corresponding to the evolving need for data-driven decision-making. The increasing patterns of claims fraud propel the demand for these techniques.
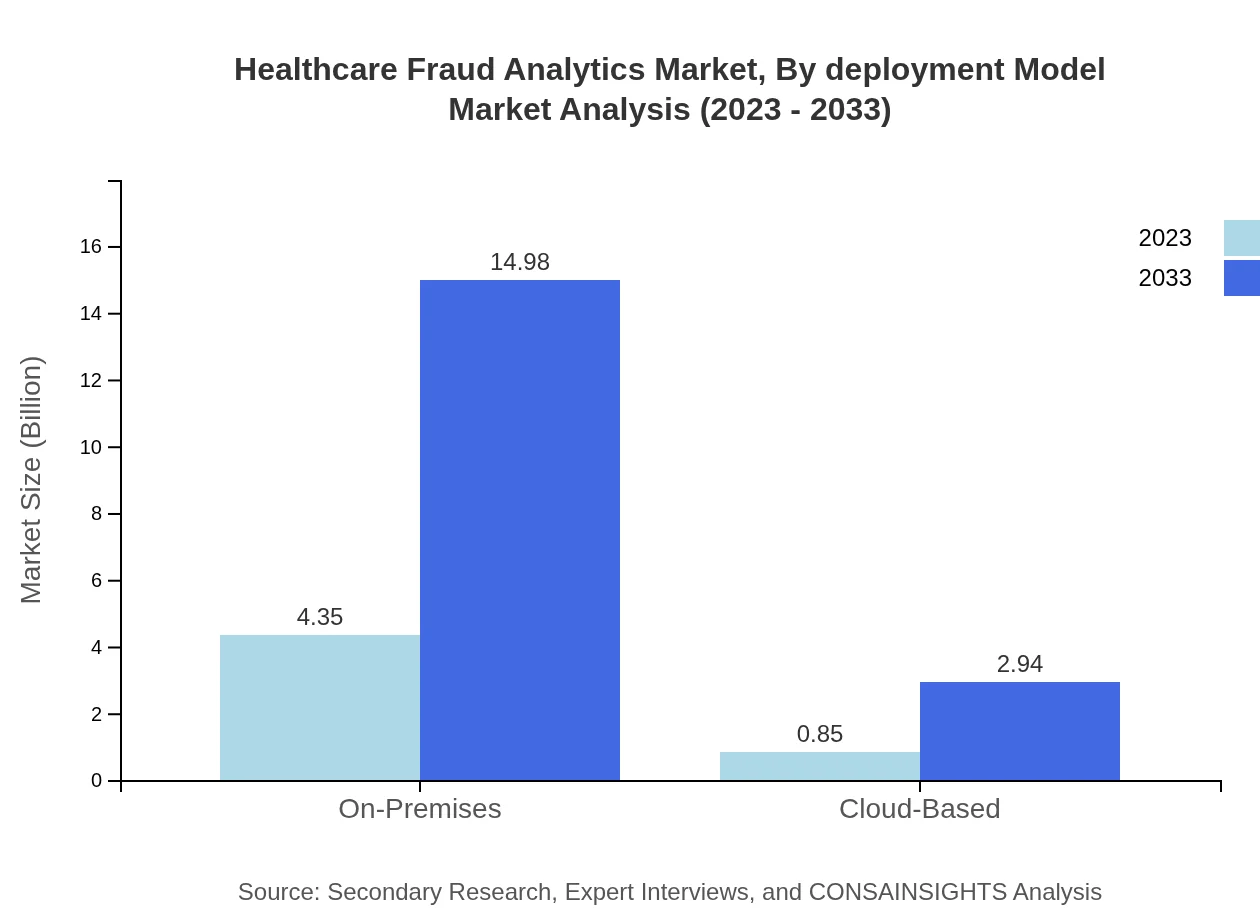
Healthcare Fraud Analytics Market Analysis By Deployment Model
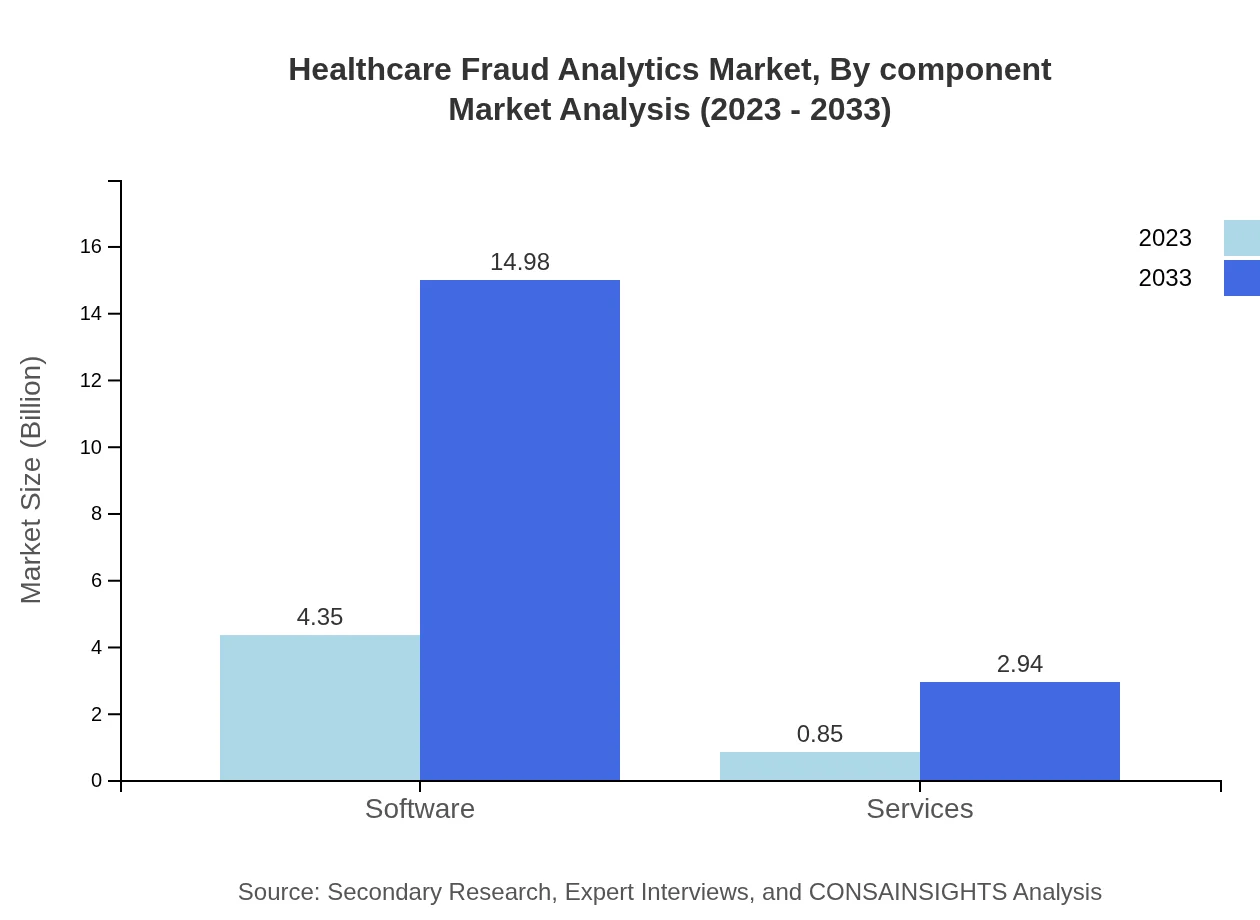
On-Premises solutions dominate with a market size of USD 4.35 billion in 2023, expected to grow to USD 14.98 billion by 2033 (83.61% market share). However, Cloud-Based solutions, at USD 0.85 billion (16.39% share) in 2023, are gaining traction as organizations look for scalable and cost-effective fraud analytics solutions.
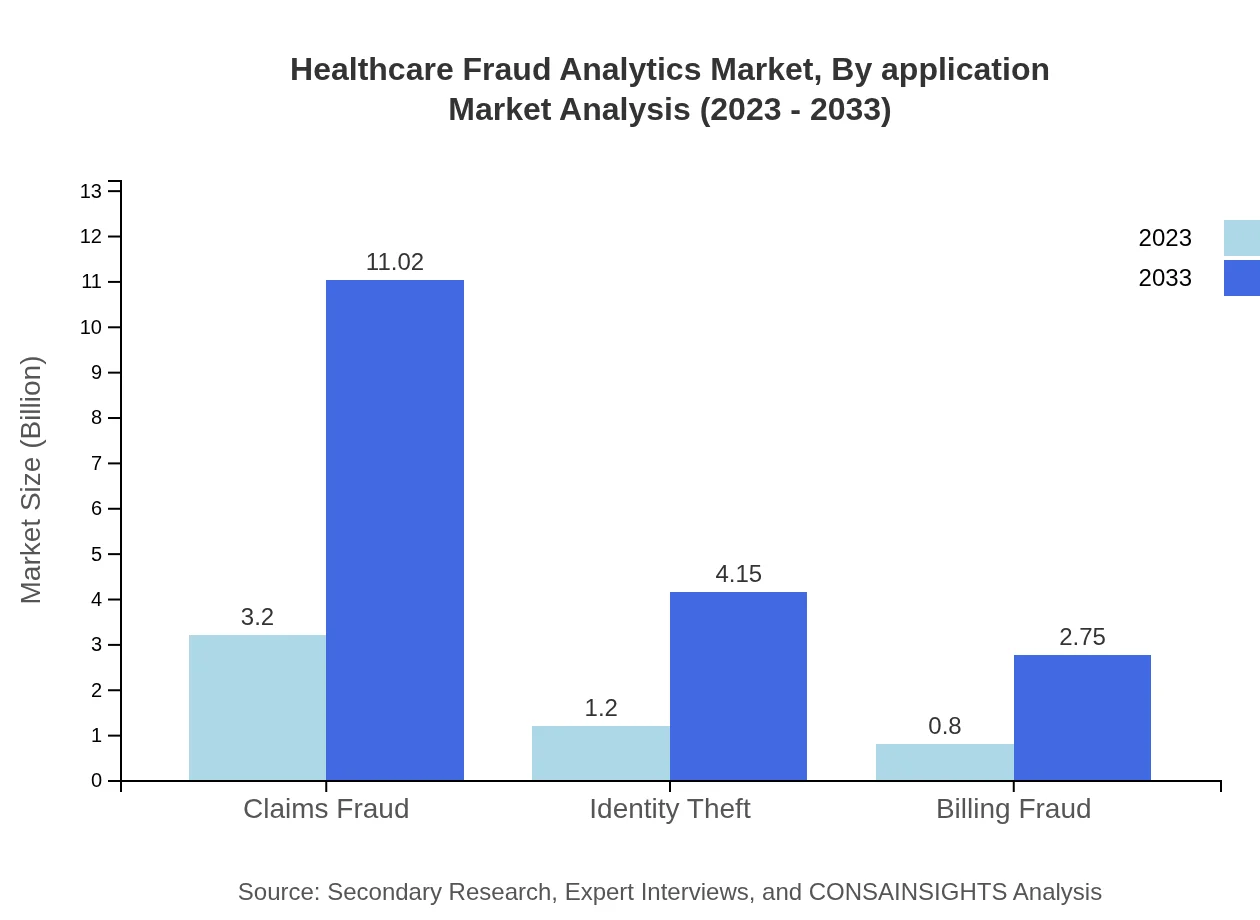
Healthcare Fraud Analytics Market Analysis By Application
Applications in Claims Fraud lead with USD 3.20 billion in 2023 to USD 11.02 billion by 2033, representing a growth reflective of the rising healthcare expenditure and fraud cases. Identity Theft and Billing Fraud are other critical applications, emphasizing the need for robust solutions across varying fraud types.
Healthcare Fraud Analytics Market Analysis By Component
Software holds a significant market share in this segment with a size of USD 4.35 billion in 2023, expected to rise to USD 14.98 billion by 2033 (83.61% share). Services contribute significantly, with expected growth from USD 0.85 billion (16.39% share) in 2023.
Healthcare Fraud Analytics Market Trends and Future Forecast
Tell us your focus area and get a customized research report.
Global Market Leaders and Top Companies in Healthcare Fraud Analytics Industry
IBM Corporation:
IBM is a leader in advanced analytics solutions, offering innovative software and consulting services to help healthcare organizations detect and prevent fraud effectively.Optum Inc.:
Optum provides healthcare analytics services focused on fraud prevention, delivering solutions customized to healthcare payers and providers.Cognizant Technology Solutions:
Cognizant delivers advanced fraud analytics solutions combined with industry expertise in the healthcare domain, enabling clients to combat fraud successfully.SAS Institute Inc.:
SAS is well-known for its robust analytics platforms, empowering healthcare organizations with predictive capabilities for fraud detection and risk management.HCL Technologies:
HCL offers comprehensive fraud analytics solutions aimed at healthcare payers, leveraging its technological expertise to enhance detection capabilities.We're grateful to work with incredible clients.









FAQs
What is the market size of healthcare Fraud Analytics?
The healthcare fraud analytics market is projected to grow from $5.2 billion in 2023 to significant heights by 2033, with a compound annual growth rate (CAGR) of 12.6%, indicating strong momentum in combating healthcare fraud.
What are the key market players or companies in this healthcare Fraud Analytics industry?
Key players in healthcare fraud analytics include major health insurers and software companies that specialize in data analytics and fraud prevention technologies. Their innovations and competitive strategies are vital for market dynamics.
What are the primary factors driving the growth in the healthcare Fraud Analytics industry?
The growth of healthcare fraud analytics is primarily driven by the increasing prevalence of healthcare fraud, regulatory pressures for compliance, advancements in analytics technologies, and the rising need for cost-effective healthcare solutions.
Which region is the fastest Growing in the healthcare Fraud Analytics?
North America is the fastest-growing region in healthcare fraud analytics, expanding from $1.94 billion in 2023 to $6.69 billion by 2033, driven by a strong focus on healthcare system efficiencies and fraud prevention.
Does ConsaInsights provide customized market report data for the healthcare Fraud Analytics industry?
Yes, ConsaInsights offers customized market report data tailored to specific needs within the healthcare-fraud-analytics industry, allowing clients to gain insights relevant to their strategic planning and operational needs.
What deliverables can I expect from this healthcare Fraud Analytics market research project?
Deliverables from this market research project typically include detailed reports, trend analysis, market forecasts, competitive landscape assessments, and actionable insights tailored to your business requirements in the healthcare fraud analytics sector.
What are the market trends of healthcare Fraud Analytics?
Current trends in the healthcare fraud analytics market include a shift towards cloud-based solutions, an emphasis on predictive analytics, increasing adoption of advanced machine learning techniques, and a growing collaboration between public and private sectors.