Healthcare Fraud Detection Market Report
Published Date: 31 January 2026 | Report Code: healthcare-fraud-detection
Healthcare Fraud Detection Market Size, Share, Industry Trends and Forecast to 2033
This report analyzes the Healthcare Fraud Detection market, providing insights into its growth, segmentation, and regional dynamics from 2023 to 2033. It offers data-driven analyses of market trends and forecasts to facilitate informed decision-making for stakeholders.
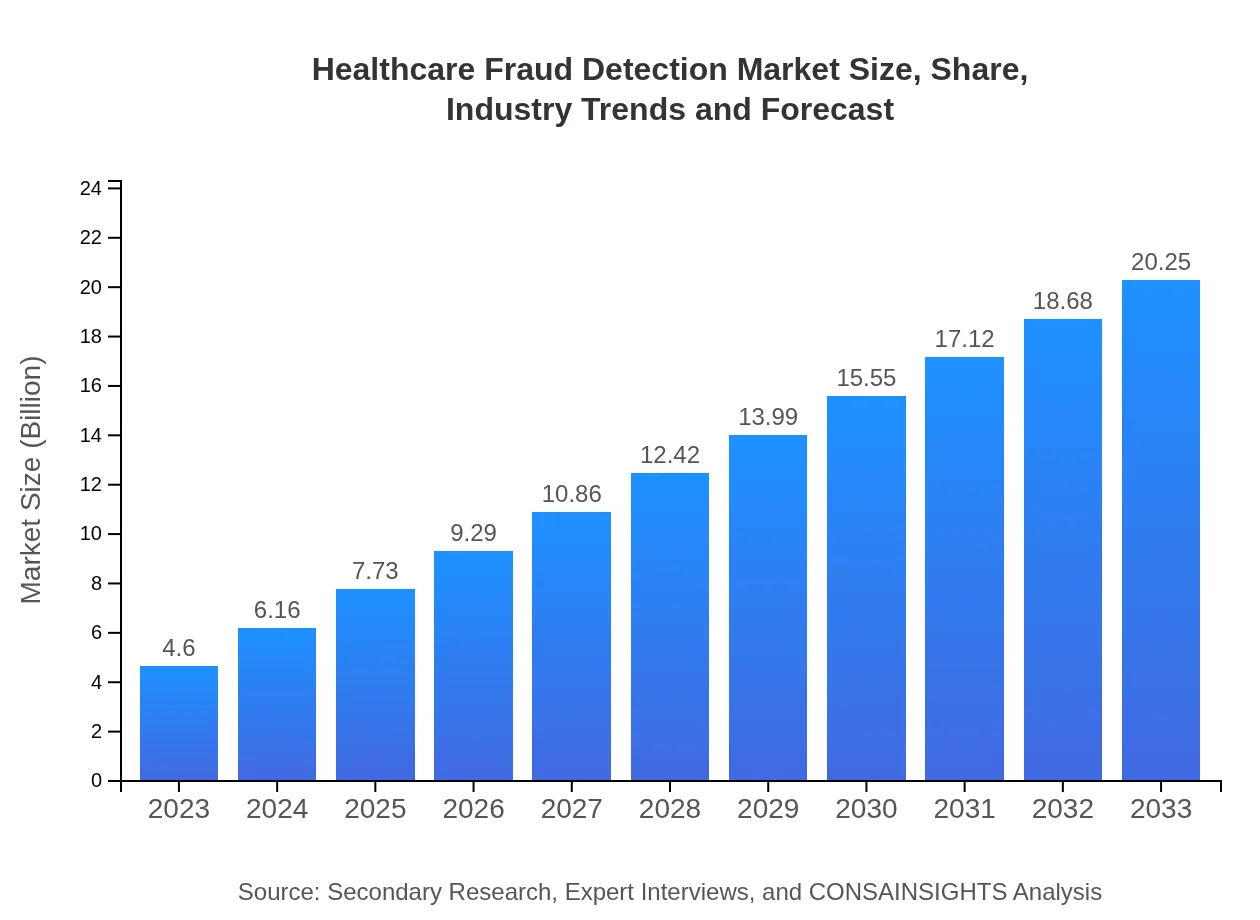
| Metric | Value |
|---|---|
| Study Period | 2023 - 2033 |
| 2023 Market Size | $4.60 Billion |
| CAGR (2023-2033) | 15.2% |
| 2033 Market Size | $20.25 Billion |
| Top Companies | IBM Corporation, SAS Institute Inc., Optum, Inc., Honeywell International Inc. |
| Last Modified Date | 31 January 2026 |
Healthcare Fraud Detection Market Overview
Customize Healthcare Fraud Detection Market Report market research report
- ✔ Get in-depth analysis of Healthcare Fraud Detection market size, growth, and forecasts.
- ✔ Understand Healthcare Fraud Detection's regional dynamics and industry-specific trends.
- ✔ Identify potential applications, end-user demand, and growth segments in Healthcare Fraud Detection
What is the Market Size & CAGR of Healthcare Fraud Detection market in 2023?
Healthcare Fraud Detection Industry Analysis
Healthcare Fraud Detection Market Segmentation and Scope
Tell us your focus area and get a customized research report.
Healthcare Fraud Detection Market Analysis Report by Region
Europe Healthcare Fraud Detection Market Report:
Europe is witnessing growth with its market size increasing from $1.15 billion in 2023 to $5.06 billion in 2033, bolstered by stringent regulations and the need for compliance mechanisms to combat fraud in healthcare.Asia Pacific Healthcare Fraud Detection Market Report:
In the Asia Pacific region, the Healthcare Fraud Detection market is expected to grow from $0.91 billion in 2023 to $4.00 billion by 2033, showcasing a strong CAGR driven by increasing healthcare expenditures and the adoption of digital health technologies.North America Healthcare Fraud Detection Market Report:
The North American market leads significantly, expanding from $1.65 billion in 2023 to $7.26 billion in 2033. The growth is attributed to established healthcare systems, high demand for innovative fraud detection solutions, and the presence of major market players.South America Healthcare Fraud Detection Market Report:
The South American market will see growth from $0.42 billion in 2023 to approximately $1.83 billion in 2033, influenced by rising awareness of fraud in healthcare and infrastructure improvements within the healthcare sector.Middle East & Africa Healthcare Fraud Detection Market Report:
The Middle East and Africa market will grow from $0.48 billion in 2023 to $2.09 billion in 2033, driven by technology adoption in healthcare and an increasing focus on fraud prevention measures.Tell us your focus area and get a customized research report.
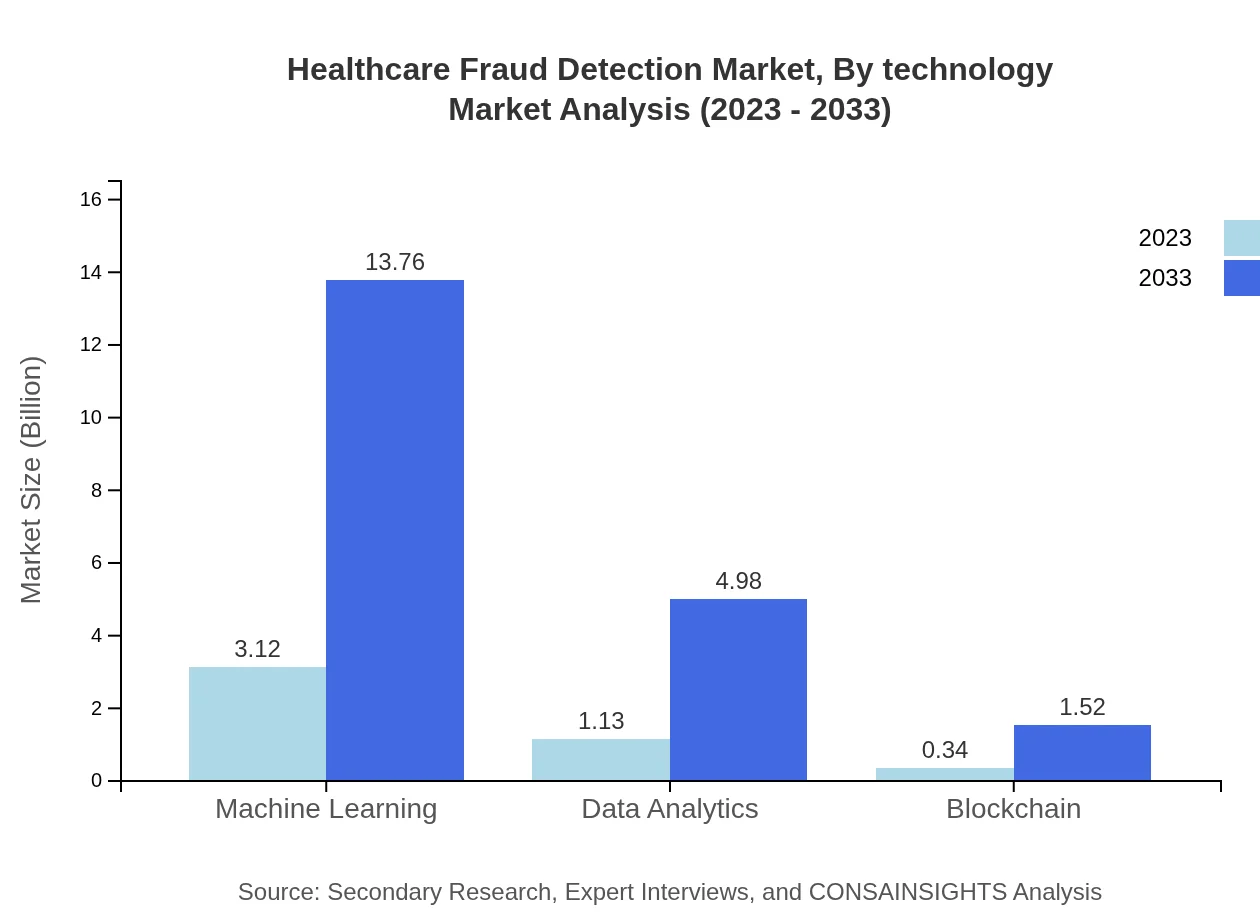
Healthcare Fraud Detection Market Analysis By Technology
The technology segment is characterized by advanced solutions such as machine learning, data analytics, and blockchain technology, crucial for enhancing fraud detection capabilities. Machine learning is projected to dominate, growing from $3.12 billion in 2023 to $13.76 billion in 2033, accounting for 67.93% market share. Data analytics will also expand from $1.13 billion to $4.98 billion, reflecting 24.58% of the market. Blockchain technology will see incremental growth, from $0.34 billion in 2023 to $1.52 billion in 2033, with a 7.49% share.
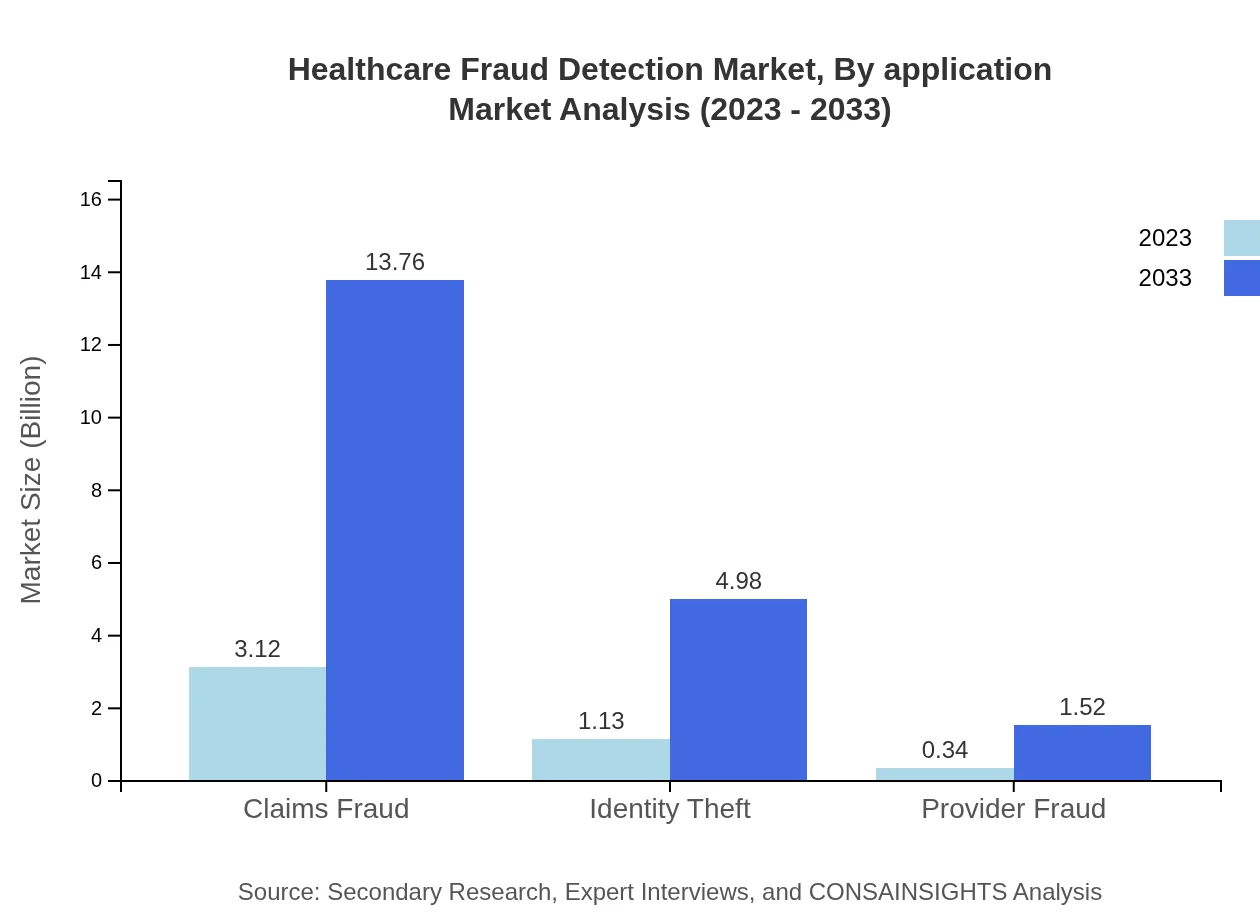
Healthcare Fraud Detection Market Analysis By Application
The application segment includes claims fraud, identity theft, and provider fraud detection. Claims fraud is expected to dominate this segment, growing from $3.12 billion in 2023 to $13.76 billion in 2033, sharing 67.93% of the market. Identity theft detection is also significant, expanding from $1.13 billion to $4.98 billion, capturing 24.58% market share, while provider fraud detection will grow from $0.34 billion in 2023 to $1.52 billion in 2033, contributing 7.49%.
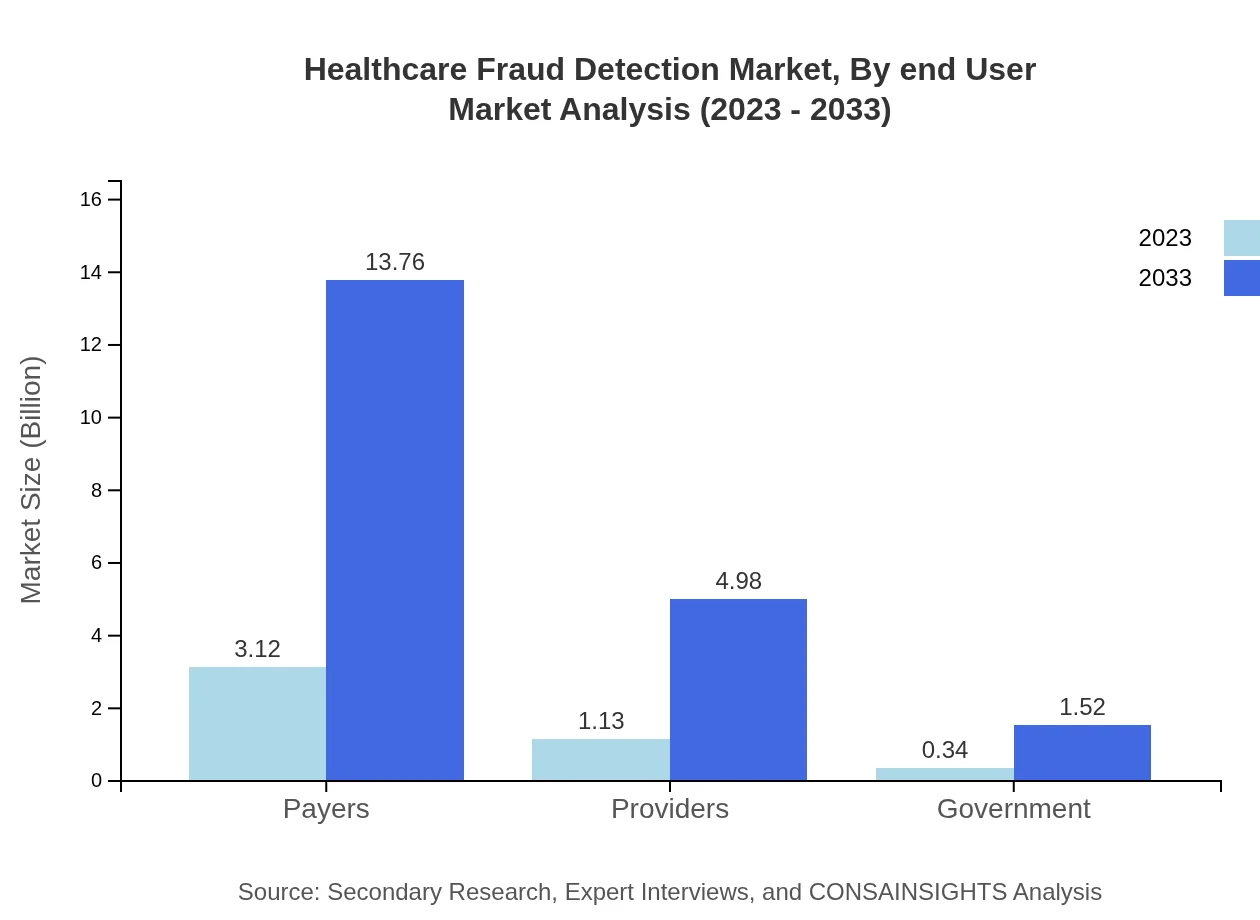
Healthcare Fraud Detection Market Analysis By End User
In the end-user segmentation, payers represent the largest share, increasing from $3.12 billion in 2023 to $13.76 billion by 2033, holding 67.93% share. Providers follow, growing from $1.13 billion to $4.98 billion, reflecting 24.58% market share. Government agencies will also see growth, from $0.34 billion to $1.52 billion, maintaining a share of 7.49%.
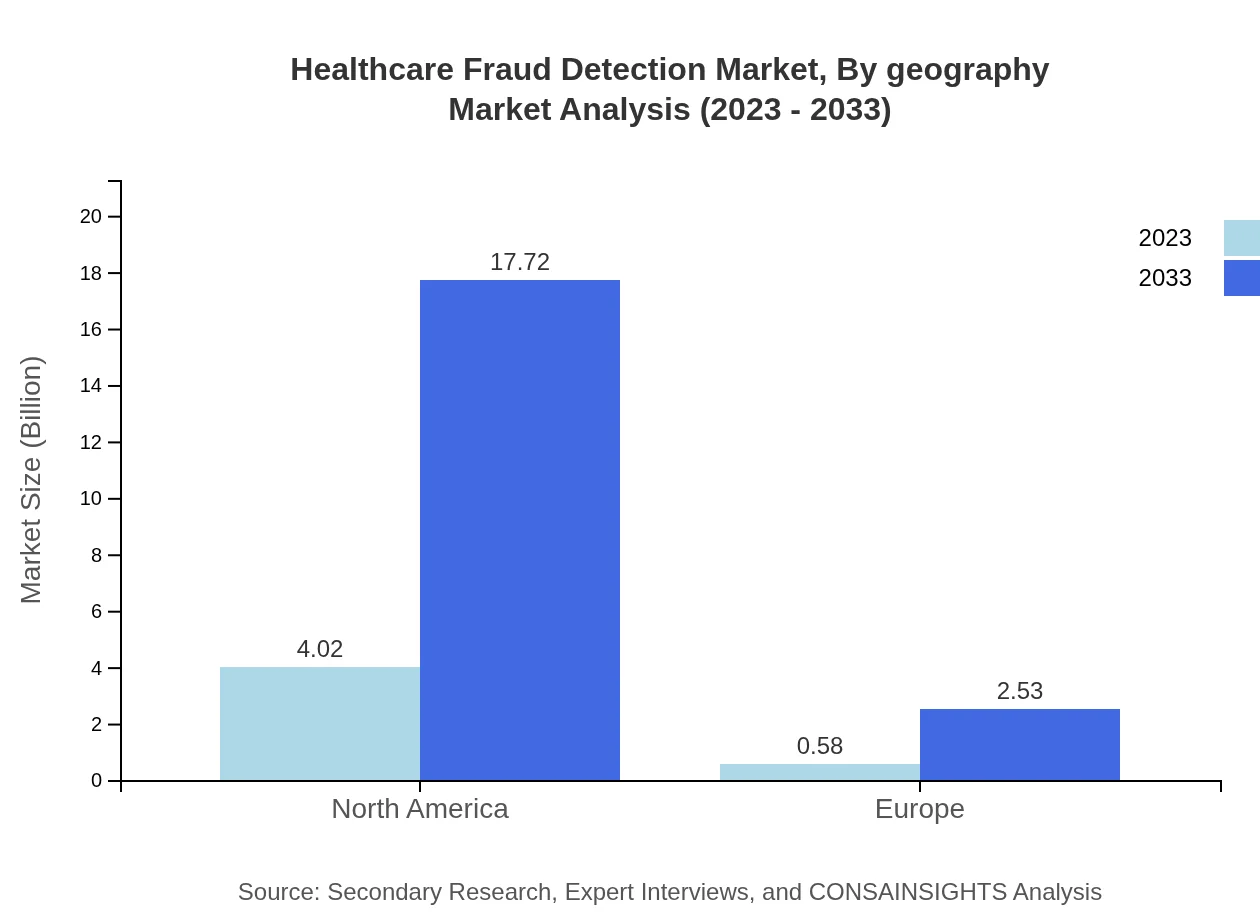
Healthcare Fraud Detection Market Analysis By Geography
This segment covers market performance across regions, demonstrating North America's dominance, where the market grows from $1.65 billion to $7.26 billion, capturing 87.49% market share. Europe follows, from $1.15 billion to $5.06 billion, representing 12.51%. The Asia Pacific region shows potential for substantial growth, with figures escalating from $0.91 billion to $4.00 billion.
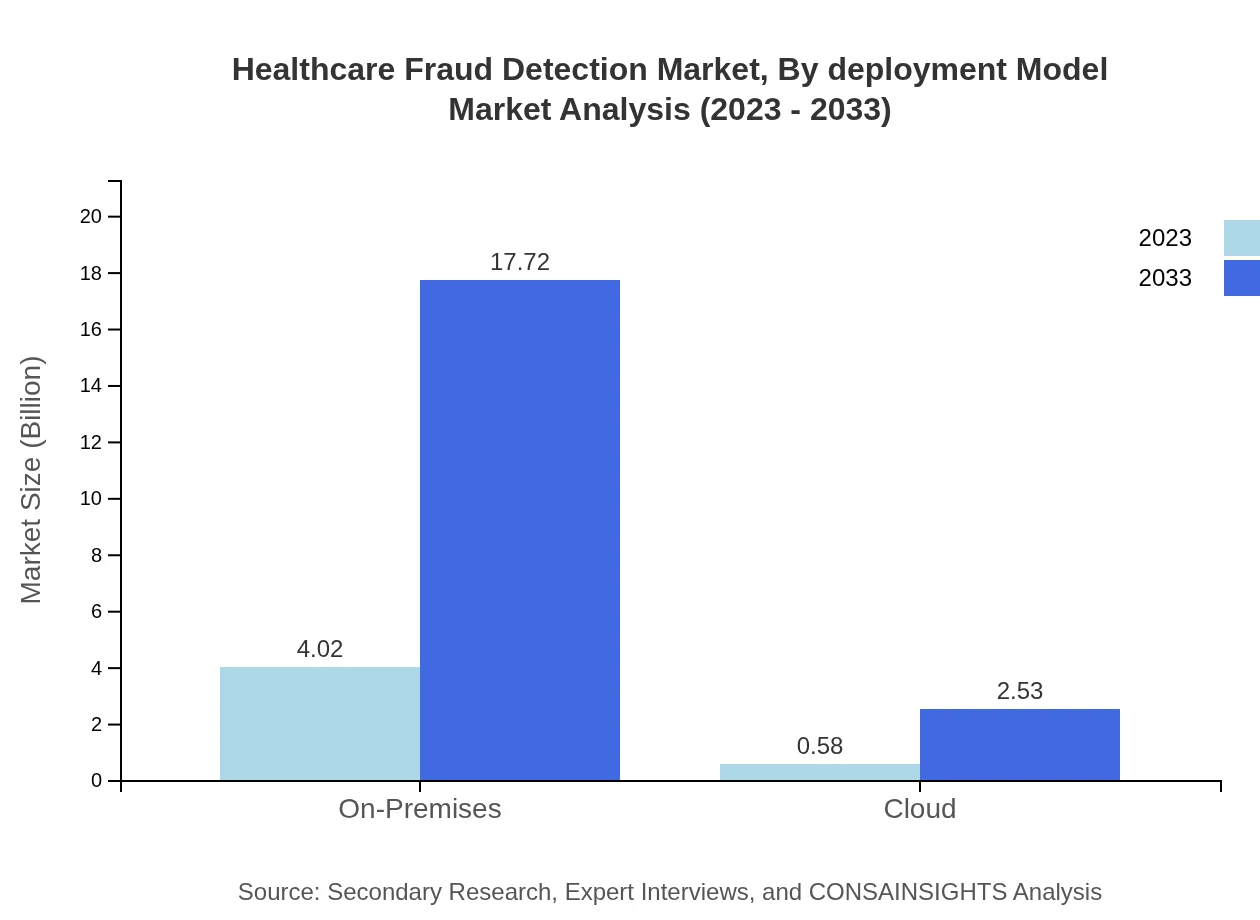
Healthcare Fraud Detection Market Analysis By Deployment Model
The deployment model segment showcases an increasing preference for the on-premises model, which grows from $4.02 billion in 2023 to $17.72 billion in 2033, securing 87.49% market share. The cloud segment will also rise, from $0.58 billion to $2.53 billion, capturing a 12.51% share, reflecting the shift towards flexible deployment options among healthcare organizations.
Healthcare Fraud Detection Market Trends and Future Forecast
Tell us your focus area and get a customized research report.
Global Market Leaders and Top Companies in Healthcare Fraud Detection Industry
IBM Corporation:
IBM offers advanced analytics and machine learning solutions to detect and prevent insurance fraud, enabling organizations to manage vast data efficiently.SAS Institute Inc.:
SAS specializes in advanced analytics and provides fraud detection solutions widely used across the healthcare industry.Optum, Inc.:
A leading health services company that leverages data analytics for fraud detection and abuse prevention within healthcare systems.Honeywell International Inc.:
Honeywell's technology focuses on integrating AI and IoT for improving fraud detection in healthcare processes.We're grateful to work with incredible clients.









FAQs
What is the market size of healthcare Fraud Detection?
The healthcare fraud detection market is valued at $4.6 billion in 2023, with a projected CAGR of 15.2% from 2023 to 2033. This significant growth reflects the increasing need for effective fraud detection solutions in the healthcare sector.
What are the key market players or companies in this healthcare Fraud Detection industry?
Key players in the healthcare fraud detection industry include companies like Verisk Analytics, ESS Protect, and SAS Institute. These organizations are pivotal in driving technological advancements and implementing robust fraud detection methodologies.
What are the primary factors driving the growth in the healthcare Fraud Detection industry?
Factors driving growth include the rising incidence of healthcare fraud, increasing regulatory pressure, advancements in technology like machine learning, and a growing emphasis on data analytics to enhance fraud detection capabilities.
Which region is the fastest Growing in the healthcare Fraud Detection?
The fastest-growing region in the healthcare fraud detection market is Asia Pacific, with a growth from $0.91 billion in 2023 to $4.00 billion by 2033, reflecting increasing healthcare infrastructure and fraud awareness in the region.
Does ConsaInsights provide customized market report data for the healthcare Fraud Detection industry?
Yes, ConsaInsights offers customized market report data tailored to specific needs in the healthcare fraud detection industry, enabling clients to obtain insights that align with their strategic initiatives and market challenges.
What deliverables can I expect from this healthcare Fraud Detection market research project?
Expect deliverables such as comprehensive market analysis, data segmentation by region and type, trend forecasting, insights on competitive landscape, and actionable recommendations to enhance market positioning.
What are the market trends of healthcare Fraud Detection?
Current trends include the adoption of machine learning technologies, increased focus on real-time fraud detection systems, growing partnership collaborations among stakeholders, and the shift towards cloud-based solutions for scalability and efficiency.