Healthcare Payer Network Management Market Report
Published Date: 31 January 2026 | Report Code: healthcare-payer-network-management
Healthcare Payer Network Management Market Size, Share, Industry Trends and Forecast to 2033
This report provides a comprehensive analysis of the Healthcare Payer Network Management market, covering current trends, market size forecasts, and regional insights from 2023 to 2033. Key data points, industry challenges, and competitive landscapes are also discussed to equip stakeholders with valuable insights.
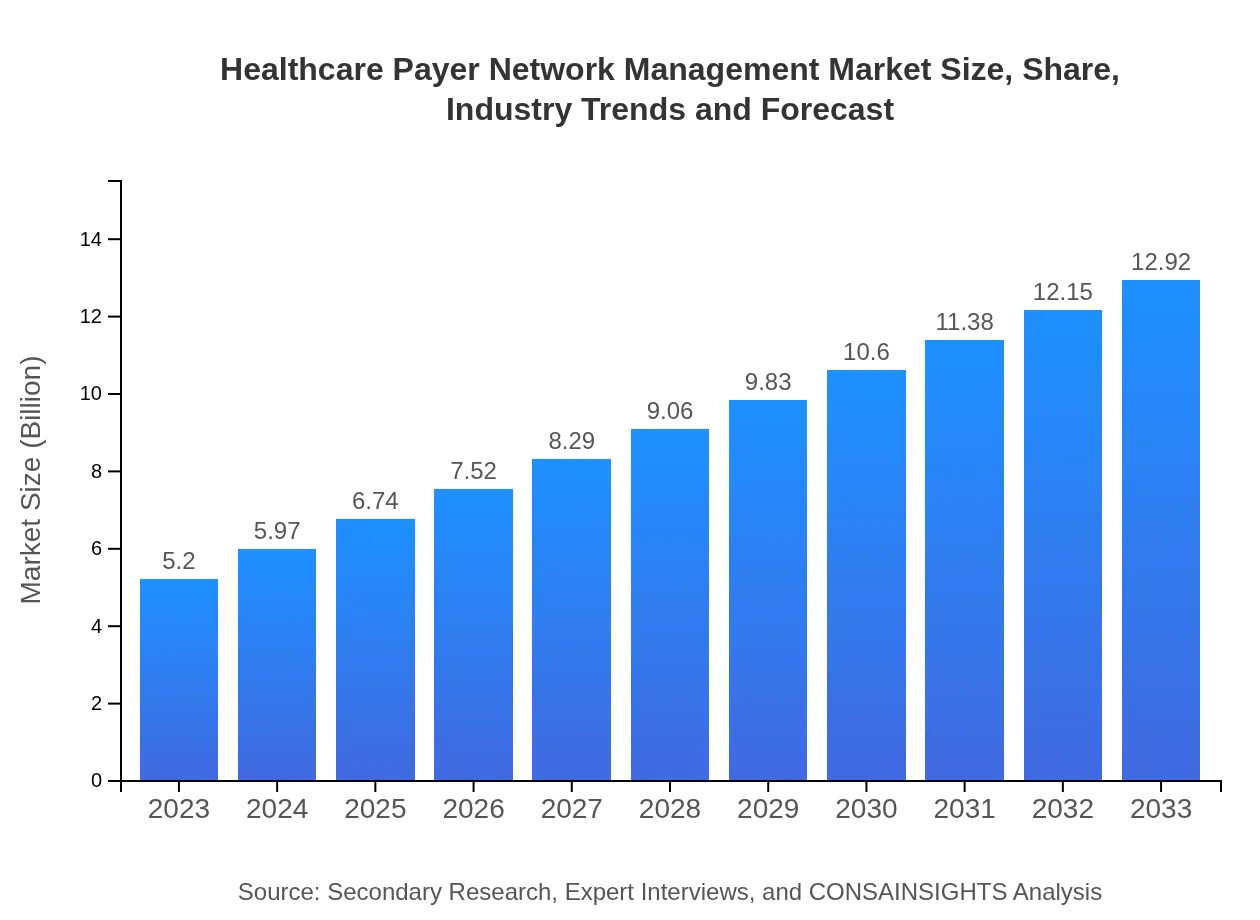
| Metric | Value |
|---|---|
| Study Period | 2023 - 2033 |
| 2023 Market Size | $5.20 Billion |
| CAGR (2023-2033) | 9.2% |
| 2033 Market Size | $12.92 Billion |
| Top Companies | UnitedHealth Group, Anthem, Inc., Cigna, Humana Inc., Molina Healthcare |
| Last Modified Date | 31 January 2026 |
Healthcare Payer Network Management Market Overview
Customize Healthcare Payer Network Management Market Report market research report
- ✔ Get in-depth analysis of Healthcare Payer Network Management market size, growth, and forecasts.
- ✔ Understand Healthcare Payer Network Management's regional dynamics and industry-specific trends.
- ✔ Identify potential applications, end-user demand, and growth segments in Healthcare Payer Network Management
What is the Market Size & CAGR of Healthcare Payer Network Management market in 2023?
Healthcare Payer Network Management Industry Analysis
Healthcare Payer Network Management Market Segmentation and Scope
Tell us your focus area and get a customized research report.
Healthcare Payer Network Management Market Analysis Report by Region
Europe Healthcare Payer Network Management Market Report:
The European Healthcare Payer Network Management market is estimated to expand from $1.33 billion in 2023 to $3.30 billion by 2033. The growth is driven by increased investment in healthcare technology, regulatory mandates for better patient data management, and rising consumer demand for care coordination.Asia Pacific Healthcare Payer Network Management Market Report:
In the Asia Pacific region, the market for Healthcare Payer Network Management is projected to grow from $1.06 billion in 2023 to $2.63 billion by 2033, driven by improving healthcare infrastructure, increasing adoption of digital health technologies, and rising investments from both public and private sectors in healthcare.North America Healthcare Payer Network Management Market Report:
In North America, particularly the United States, the market will grow significantly from $1.82 billion in 2023 to $4.51 billion in 2033. This growth is attributed to a higher emphasis on value-based care models, regulatory pressures, and the ongoing digitization of healthcare operations.South America Healthcare Payer Network Management Market Report:
The South American market is anticipated to expand from $0.38 billion in 2023 to $0.95 billion by 2033. Key growth drivers include a rising focus on healthcare reforms and increased demand for efficient payer-provider networks to enhance patient care delivery amidst economic challenges.Middle East & Africa Healthcare Payer Network Management Market Report:
The Middle East and Africa market is expected to see growth from $0.61 billion in 2023 to $1.52 billion by 2033, stimulated by rising healthcare expenditure, government initiatives to improve healthcare delivery, and the increased use of technology in managing payer networks.Tell us your focus area and get a customized research report.
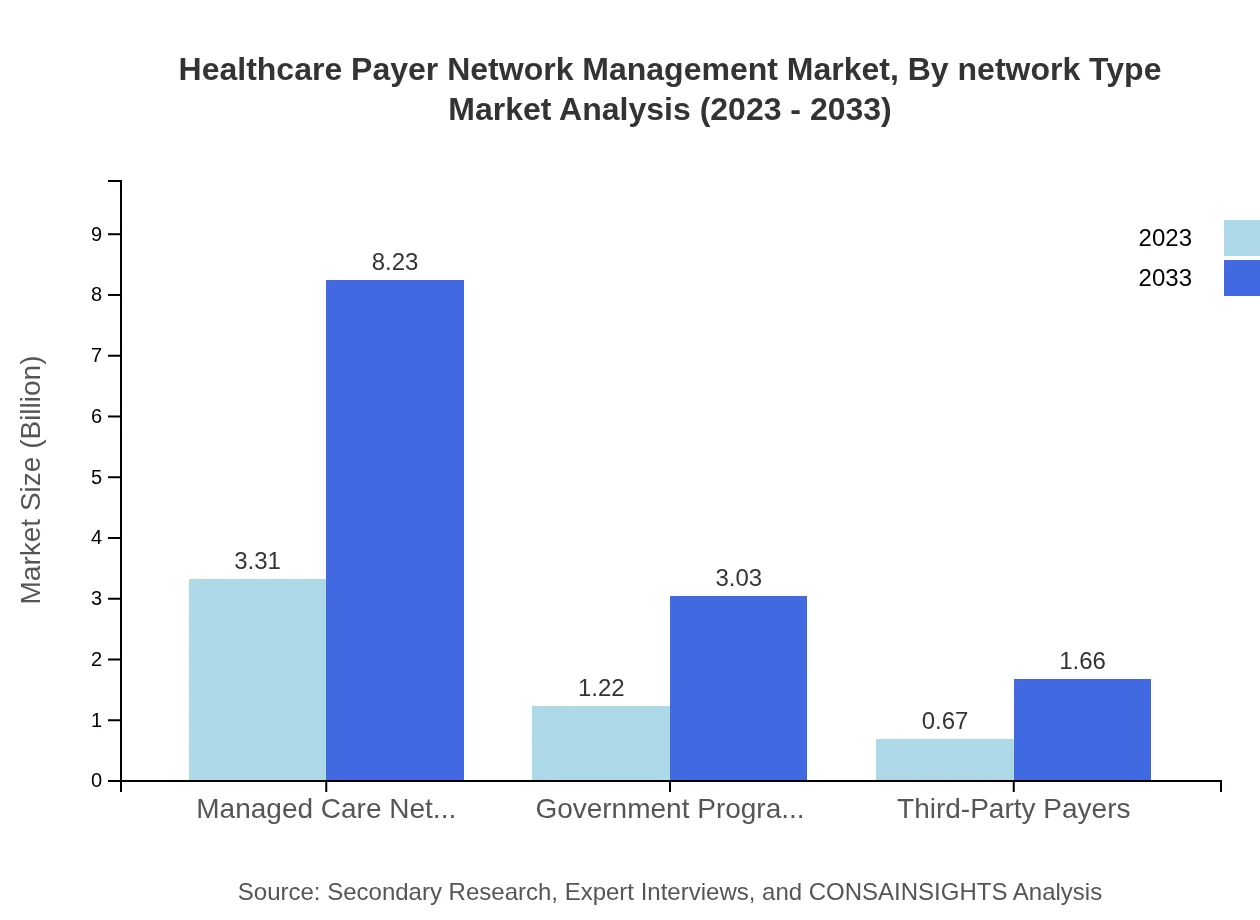
Healthcare Payer Network Management Market Analysis By Network Type
The segment of managed care networks dominates the market with a size of $3.31 billion in 2023, expected to grow to $8.23 billion by 2033. This segment holds a market share of approximately 63.68%, reflecting the critical importance of managed care in optimizing healthcare provision.
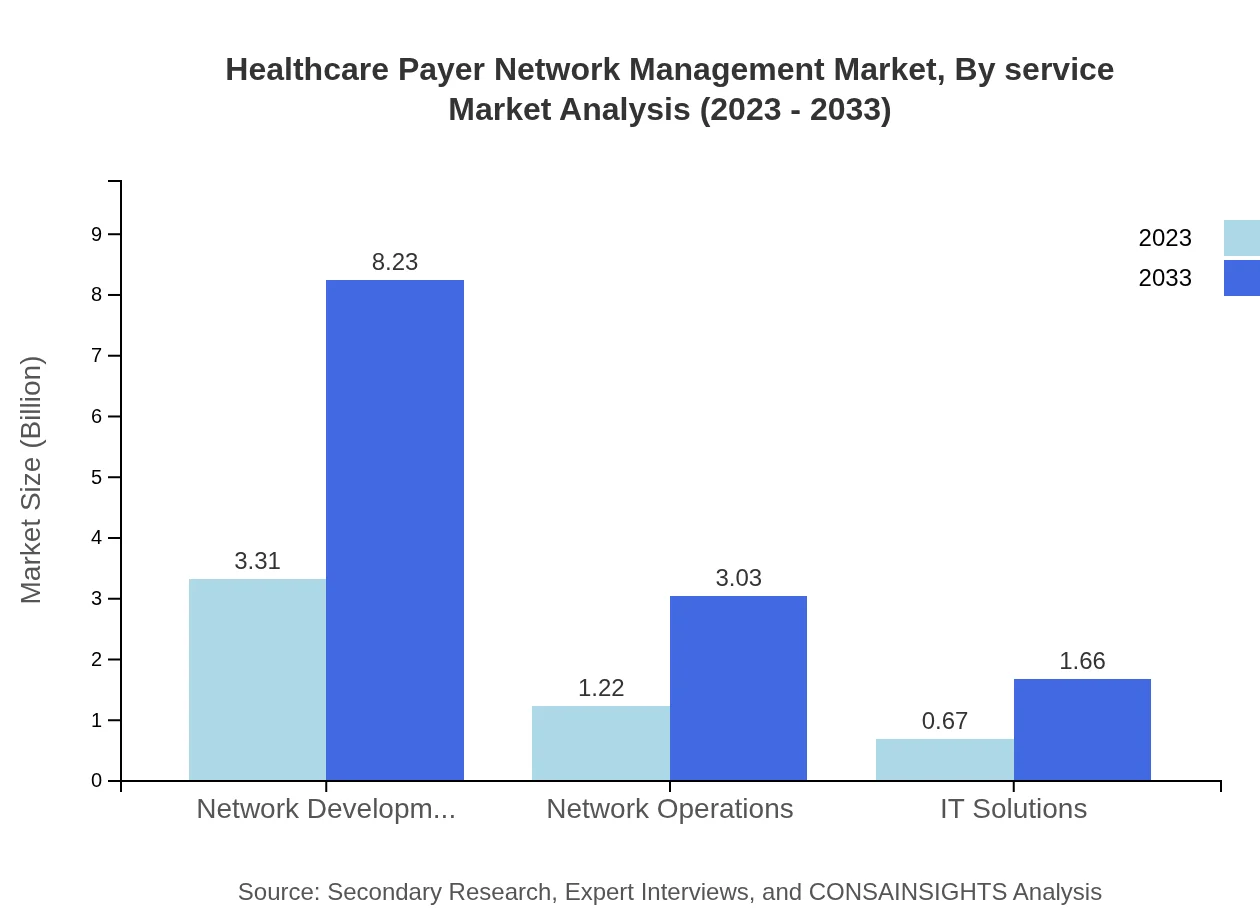
Healthcare Payer Network Management Market Analysis By Service
Analytics and IT solutions are pivotal in this market, with analytics showcasing a size of $3.31 billion in 2023 and projected to maintain a steady state with a 63.68% share of the market, reflecting their crucial role in enhancing decision-making and operational outcomes.
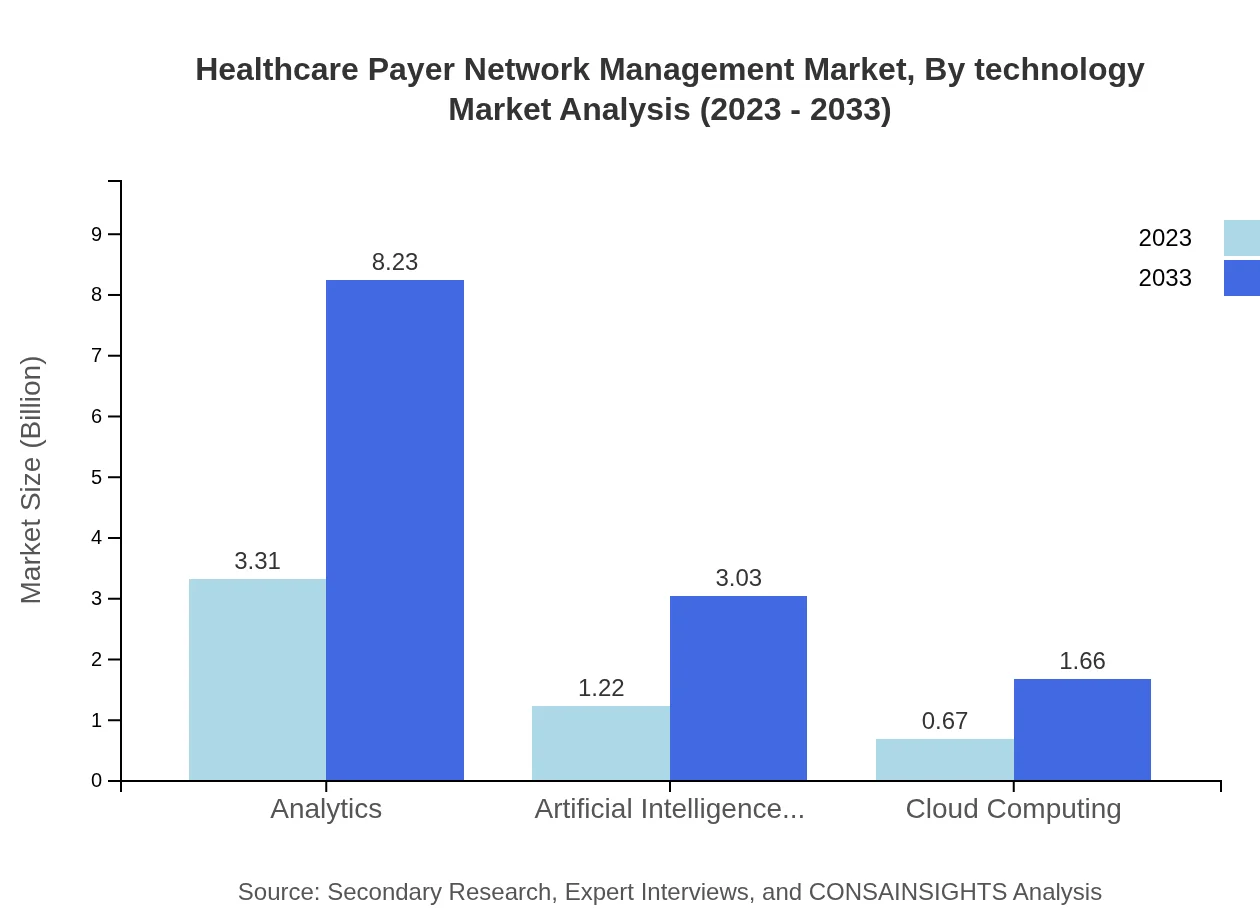
Healthcare Payer Network Management Market Analysis By Technology
AI and ML technologies in the healthcare payer market are set to grow from $1.22 billion in size in 2023 to $3.03 billion by 2033, with a notable market share of 23.49%, underscoring the growing reliance on predictive analytics to drive efficiencies.
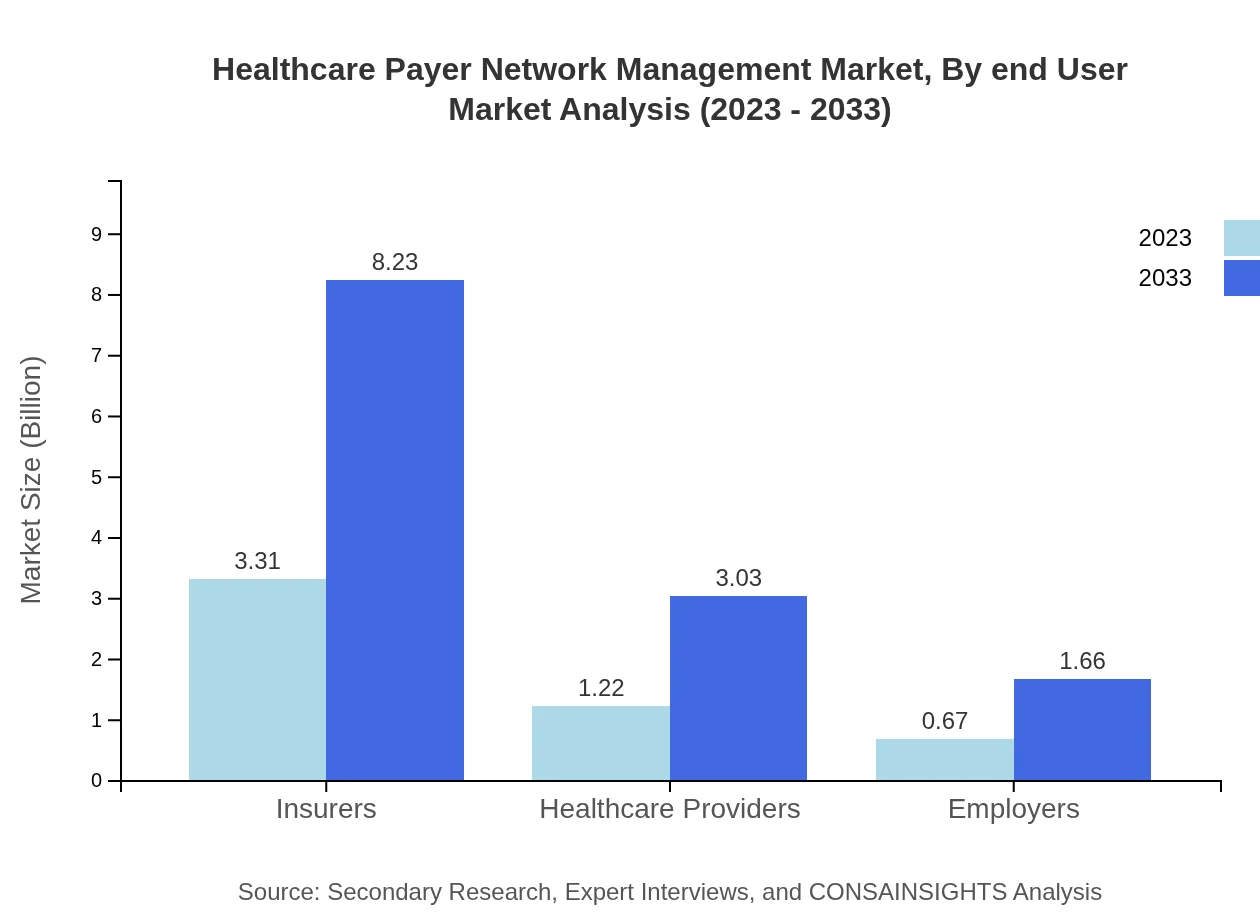
Healthcare Payer Network Management Market Analysis By End User
The end-user segment showcases insurers as dominating players, with market size growth from $3.31 billion in 2023 to $8.23 billion by 2033. Insurers hold 63.68% of market share, highlighting their imperative role in the network management landscape.
Healthcare Payer Network Management Market Trends and Future Forecast
Tell us your focus area and get a customized research report.
Global Market Leaders and Top Companies in Healthcare Payer Network Management Industry
UnitedHealth Group:
One of the largest healthcare companies globally, UnitedHealth Group provides comprehensive health management solutions, leveraging advanced analytics and IT services.Anthem, Inc.:
Anthem is a health insurance provider that uses innovative technologies to improve health management solutions for payers and healthcare providers.Cigna:
Cigna offers health services and payer management solutions, focusing on integrated care models and enhanced patient engagement.Humana Inc.:
Humana specializes in integrated healthcare services and payer networks, leading advancements in value-based care models.Molina Healthcare:
Molina supports government programs and offers innovative solutions to manage payer networks efficiently, with a substantial impact in the Medicaid segment.We're grateful to work with incredible clients.








FAQs
What is the market size of healthcare Payer Network Management?
The healthcare payer network management market is valued at approximately $5.2 billion in 2023 and is projected to grow at a CAGR of 9.2% until 2033.
What are the key market players or companies in this healthcare payer network management industry?
Key players include major healthcare insurers, IT solution providers, and network management platforms that specialize in payer relationships and operational efficiencies.
What are the primary factors driving the growth in the healthcare payer network management industry?
Growth is driven by rising healthcare costs, the need for efficient claims processing, and the increasing adoption of IT solutions that enhance network management capabilities.
Which region is the fastest Growing in the healthcare payer network management?
North America is the fastest-growing region, projected to expand from $1.82 billion in 2023 to $4.51 billion by 2033, leveraging advanced technology and healthcare reforms.
Does ConsaInsights provide customized market report data for the healthcare payer network management industry?
Yes, ConsaInsights offers customized market research reports tailored to specific needs within the healthcare payer network management sector.
What deliverables can I expect from this healthcare payer network management market research project?
Deliverables include comprehensive market analysis, regional insights, competitive landscape assessments, and future growth trends over the forecast period.
What are the market trends of healthcare payer network management?
Current trends include increased reliance on analytics, AI integration, telehealth expansion, and a shift towards value-based care models.