Healthcare Provider Network Management Market Report
Published Date: 31 January 2026 | Report Code: healthcare-provider-network-management
Healthcare Provider Network Management Market Size, Share, Industry Trends and Forecast to 2033
This market report provides an in-depth analysis of the Healthcare Provider Network Management sector, covering market size, trends, and forecasts from 2023 to 2033. It highlights insights across various segments, regional markets, industry dynamics, and key players influencing the landscape.
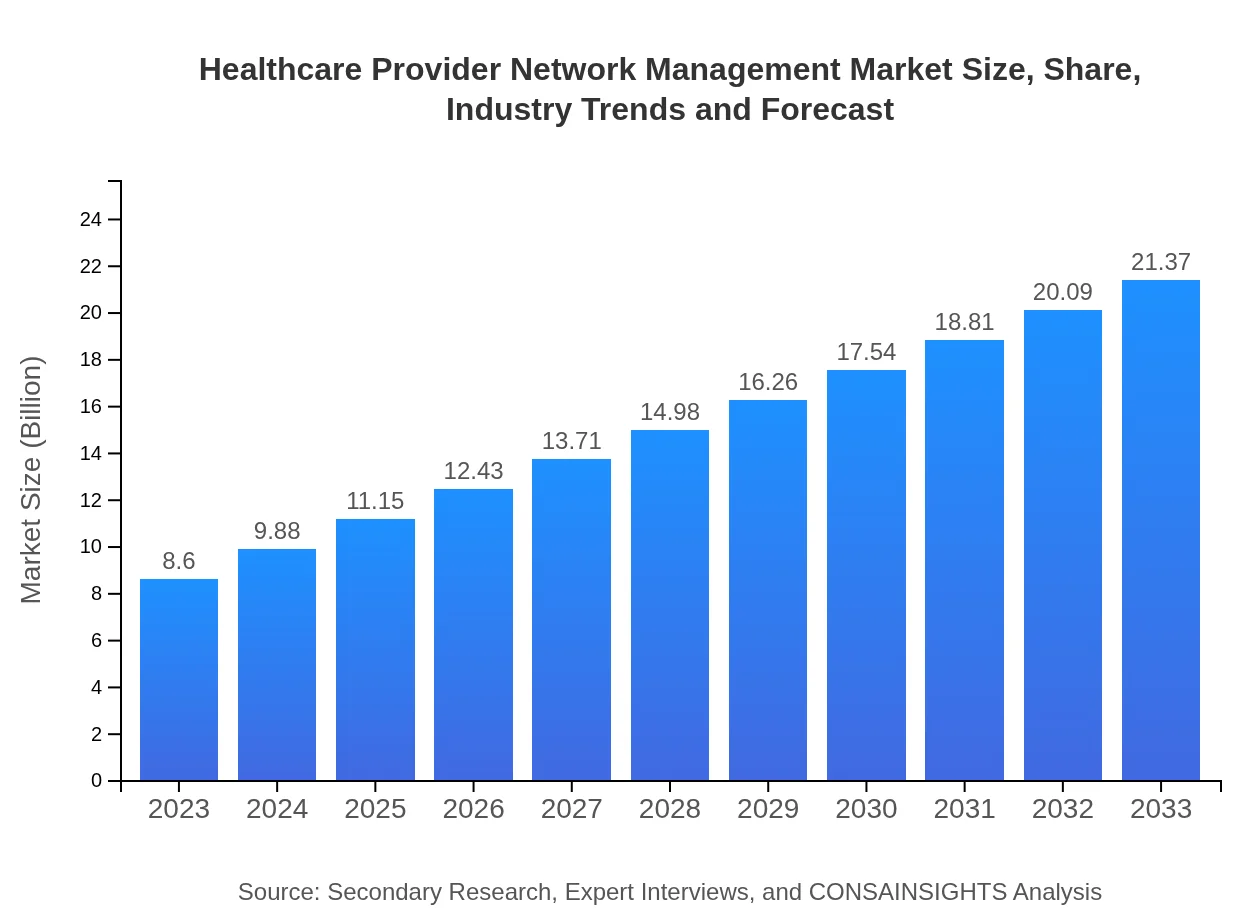
| Metric | Value |
|---|---|
| Study Period | 2023 - 2033 |
| 2023 Market Size | $8.60 Billion |
| CAGR (2023-2033) | 9.2% |
| 2033 Market Size | $21.37 Billion |
| Top Companies | Optum, McKesson Corporation, Epic Systems, Cerner Corporation, Allscripts Healthcare Solutions |
| Last Modified Date | 31 January 2026 |
Healthcare Provider Network Management Market Overview
Customize Healthcare Provider Network Management Market Report market research report
- ✔ Get in-depth analysis of Healthcare Provider Network Management market size, growth, and forecasts.
- ✔ Understand Healthcare Provider Network Management's regional dynamics and industry-specific trends.
- ✔ Identify potential applications, end-user demand, and growth segments in Healthcare Provider Network Management
What is the Market Size & CAGR of Healthcare Provider Network Management market in 2023?
Healthcare Provider Network Management Industry Analysis
Healthcare Provider Network Management Market Segmentation and Scope
Tell us your focus area and get a customized research report.
Healthcare Provider Network Management Market Analysis Report by Region
Europe Healthcare Provider Network Management Market Report:
The European market for Healthcare Provider Network Management is anticipated to grow from $2.87 billion in 2023 to $7.14 billion by 2033. Increasing regulatory requirements and a push towards integrated care models are primary influencers. Countries like Germany and the UK are leading the way by implementing advanced network management systems to facilitate provider collaboration and improve patient outcomes.Asia Pacific Healthcare Provider Network Management Market Report:
The Asia Pacific region is experiencing rapid growth in the Healthcare Provider Network Management market, with a projected market size of $3.38 billion by 2033, up from $1.36 billion in 2023. The increasing adoption of digital health solutions and government initiatives to enhance healthcare delivery drive this growth. Countries like India and China are investing heavily in health IT systems, facilitating better provider management and patient care.North America Healthcare Provider Network Management Market Report:
North America holds a significant share of the Healthcare Provider Network Management market, with values expected to rise from $3.10 billion in 2023 to $7.71 billion by 2033. This dominance is driven by technological advancements, high healthcare expenditure, and a growing emphasis on data-driven decision-making in provider networks. The U.S. leads with a robust infrastructure that supports innovative management solutions.South America Healthcare Provider Network Management Market Report:
In South America, the Healthcare Provider Network Management market is forecasted to grow from $0.32 billion in 2023 to $0.79 billion by 2033. Factors such as rising healthcare demands, efforts to improve health outcomes, and the growth of public and private healthcare sectors are key drivers fueling market expansion. Countries like Brazil and Argentina are at the forefront of adopting network management solutions to optimize care delivery.Middle East & Africa Healthcare Provider Network Management Market Report:
The Middle East and Africa region is expected to see growth from $0.95 billion in 2023 to $2.35 billion by 2033. The market is supported by investments in healthcare infrastructure and initiatives to enhance the quality of care. Countries like the UAE and South Africa are witnessing significant advancements in health information systems, driving the demand for network management solutions.Tell us your focus area and get a customized research report.
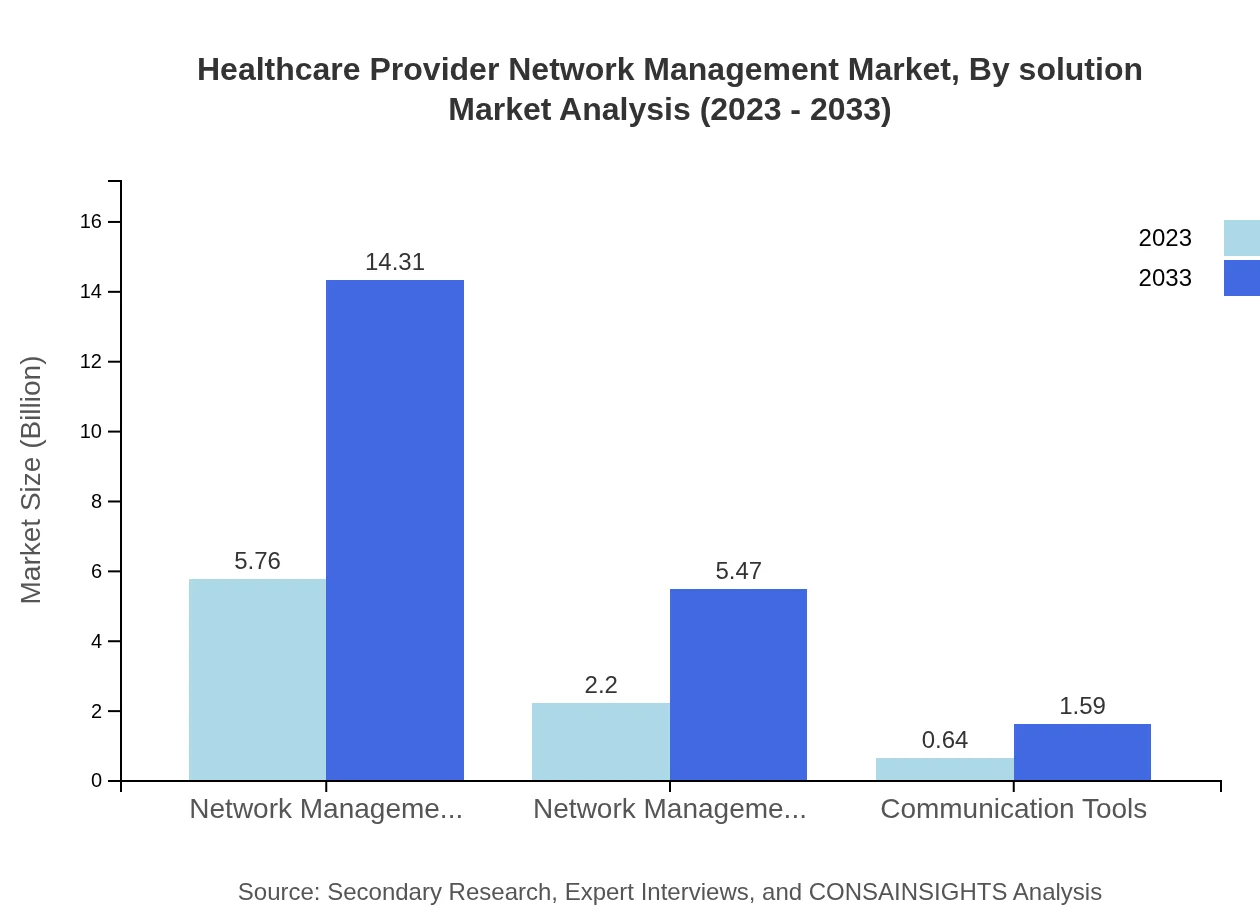
Healthcare Provider Network Management Market Analysis By Solution
The Healthcare Provider Network Management market is segmented into solutions such as network management software, network management services, and communication tools. As of 2023, network management software leads the market with a valuation of $5.76 billion, expected to grow to $14.31 billion by 2033. The software's capabilities in real-time data analysis and provider performance tracking are invaluable. Network management services, valued at $2.20 billion in 2023, will grow to $5.47 billion by 2033, while communication tools are projected to reach $1.59 billion.
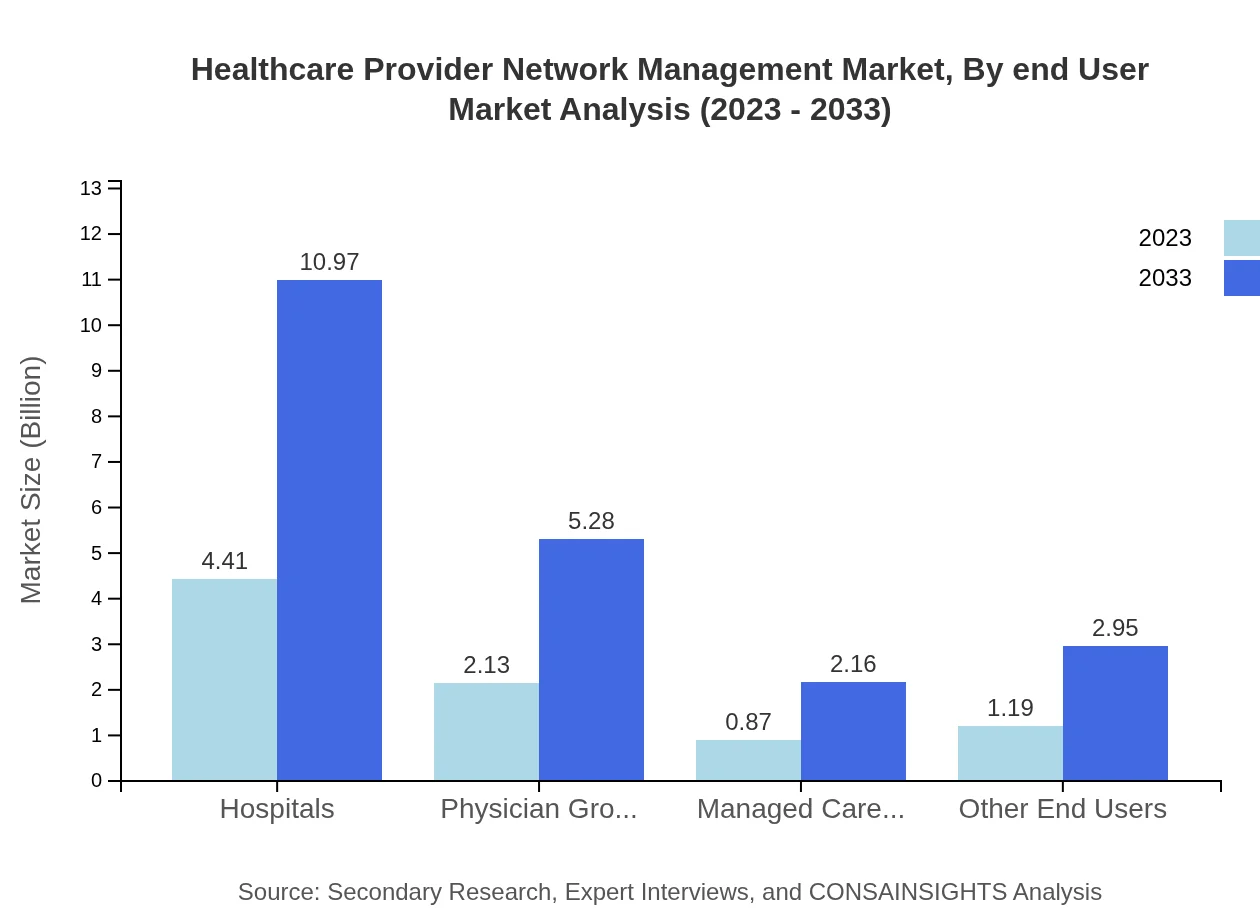
Healthcare Provider Network Management Market Analysis By End User
Market segmentation by end-users includes hospitals, physician groups, managed care organizations, and other healthcare entities. Hospitals dominate with a market size of $4.41 billion in 2023, growing to $10.97 billion by 2033 due to increased patient volumes and need for efficient management. Physician groups and managed care organizations contribute significantly as well, with market sizes projected to be $2.13 billion and $0.87 billion, respectively, in 2023.
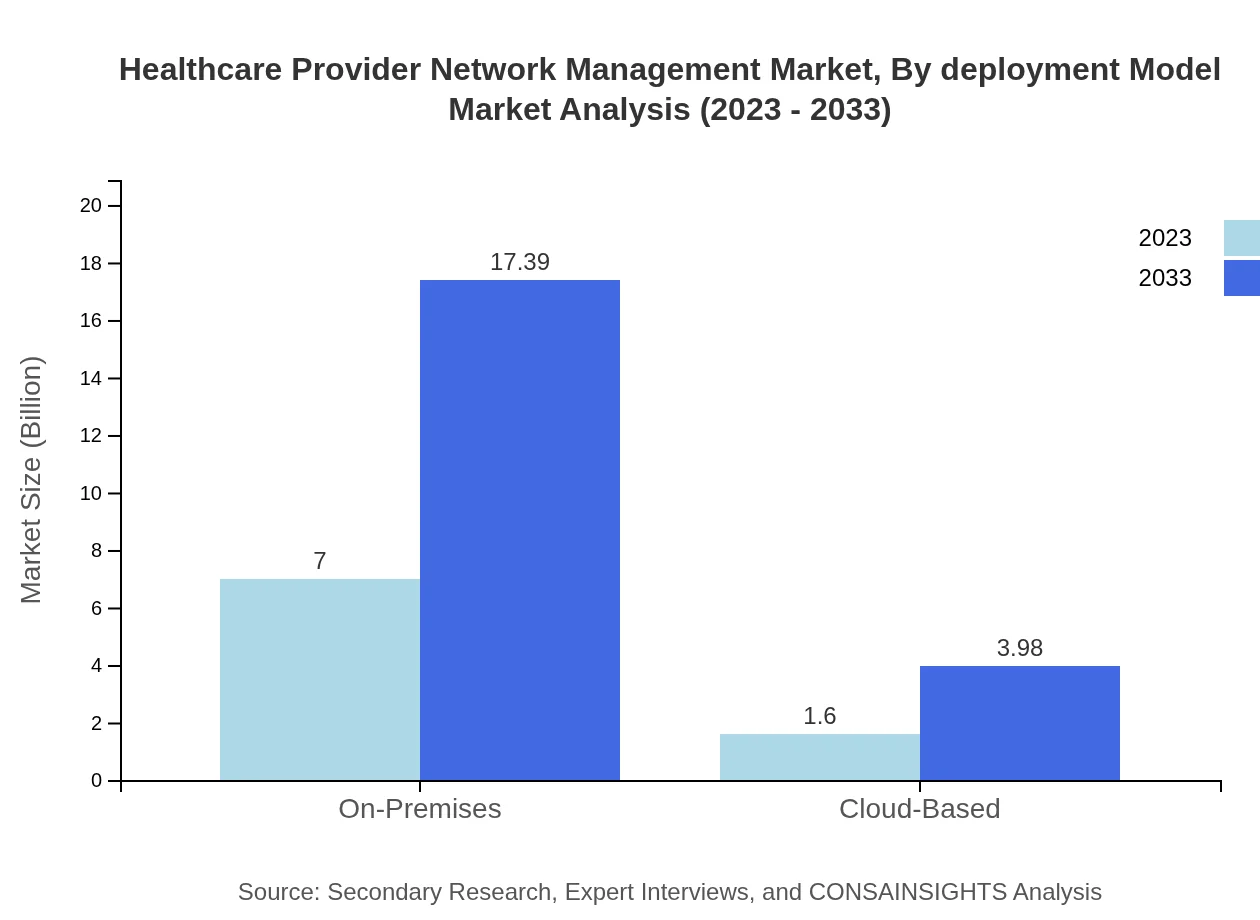
Healthcare Provider Network Management Market Analysis By Deployment Model
The market is also analyzed by deployment models, including on-premises and cloud-based solutions. On-premises solutions encompass a substantial market segment, growing from $7.00 billion in 2023 to $17.39 billion by 2033. Meanwhile, cloud-based solutions are expected to increase from $1.60 billion to $3.98 billion, driven by their flexibility and cost-effectiveness.
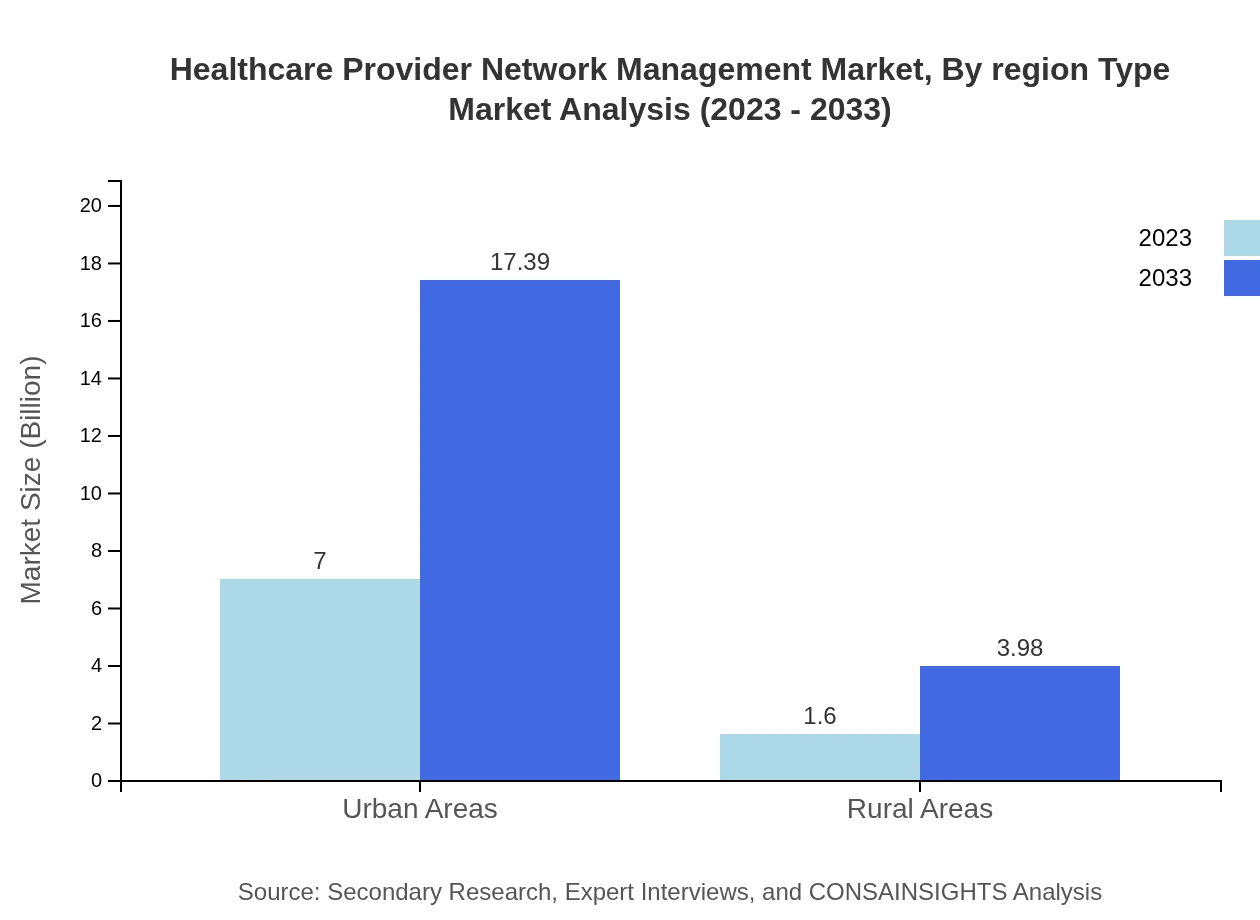
Healthcare Provider Network Management Market Analysis By Region Type
Regional analysis indicates variations in market growth driven by local healthcare policies and technological adoption. North America remains the largest market, followed by Europe and Asia Pacific. Innovations in digital health are particularly influencing growth patterns in these regions, reflecting differing priorities and levels of investment across healthcare systems.
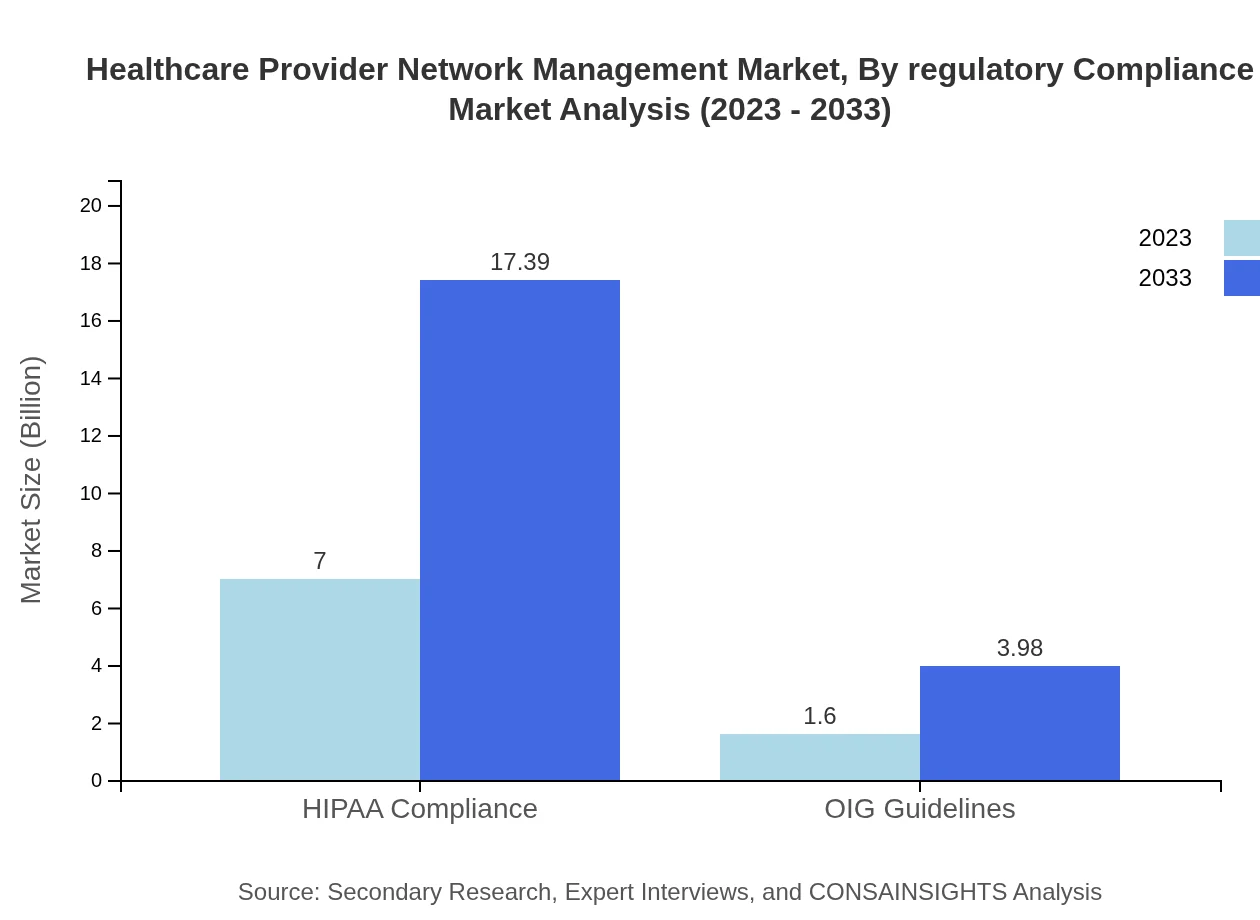
Healthcare Provider Network Management Market Analysis By Regulatory Compliance
Regulatory compliance segments include HIPAA compliance and OIG guidelines. The segment focusing on HIPAA compliance is significant, projected to maintain a robust share of approximately 81.39% of the market through 2033. Compliance with these regulations is essential for maintaining network integrity and ensuring patient confidentiality.
Healthcare Provider Network Management Market Trends and Future Forecast
Tell us your focus area and get a customized research report.
Global Market Leaders and Top Companies in Healthcare Provider Network Management Industry
Optum:
A leading health services and information technology company that provides innovative healthcare solutions, including advanced provider network management systems.McKesson Corporation:
A major supplier of healthcare management software and services, McKesson offers solutions that enhance provider performance and optimize network relationships.Epic Systems:
Known for its electronic health record (EHR) solutions, Epic also provides integrated network management tools that facilitate seamless communication and collaboration among providers.Cerner Corporation:
Cerner focuses on health information technology and offers extensive solutions for managing provider networks, driving efficiency and improved patient care.Allscripts Healthcare Solutions:
Allscripts develops and delivers innovative technology solutions for healthcare organizations, including comprehensive network management systems to support care coordination.We're grateful to work with incredible clients.









FAQs
What is the market size of healthcare Provider Network Management?
The global healthcare provider network management market is currently valued at approximately $8.6 billion, with a robust CAGR of 9.2% anticipated until 2033. Regionally, significant growth is expected across various segments, indicating a thriving industry ahead.
What are the key market players or companies in the healthcare Provider Network Management industry?
Key players in the healthcare provider network management industry include companies specializing in network management software and services. These entities focus on streamlining operations, regulatory compliance, and enhancing the overall efficiency of healthcare networks.
What are the primary factors driving the growth in the healthcare Provider Network Management industry?
Growth drivers for the healthcare provider network management market include the increase in patient volume, the need for operational efficiency, advancements in technology, and the regulatory requirements for maintaining quality standards in healthcare delivery.
Which region is the fastest Growing in the healthcare Provider Network Management market?
The fastest-growing region in the healthcare provider network management market is projected to be North America, with a market growth from $3.10 billion in 2023 to $7.71 billion in 2033, accounting for substantial regional demand and technological advancements.
Does ConsaInsights provide customized market report data for the healthcare Provider Network Management industry?
Yes, ConsaInsights offers tailored market report data for the healthcare provider network management industry, allowing clients to access specific insights that meet their unique business requirements and strategic objectives.
What deliverables can I expect from this healthcare Provider Network Management market research project?
Deliverables from the healthcare provider network management market research project include detailed reports on market size, trends, growth forecasts, segment insights, and comprehensive analyses of regional performances.
What are the market trends of healthcare Provider Network Management?
Current market trends in healthcare provider network management include a shift towards cloud-based solutions, increasing importance of regulatory compliance, adoption of advanced analytics, and a growing emphasis on patient-centric network designs.