Midrevenue Cycle Management Clinical Documentation Improvement Market Report
Published Date: 31 January 2026 | Report Code: midrevenue-cycle-management-clinical-documentation-improvement
Midrevenue Cycle Management Clinical Documentation Improvement Market Size, Share, Industry Trends and Forecast to 2033
This report delves into the Midrevenue Cycle Management Clinical Documentation Improvement market, examining trends, sizes, and forecasts from 2023 to 2033. It offers data-driven insights while analyzing regional dynamics, technological advancements, and market segmentation.
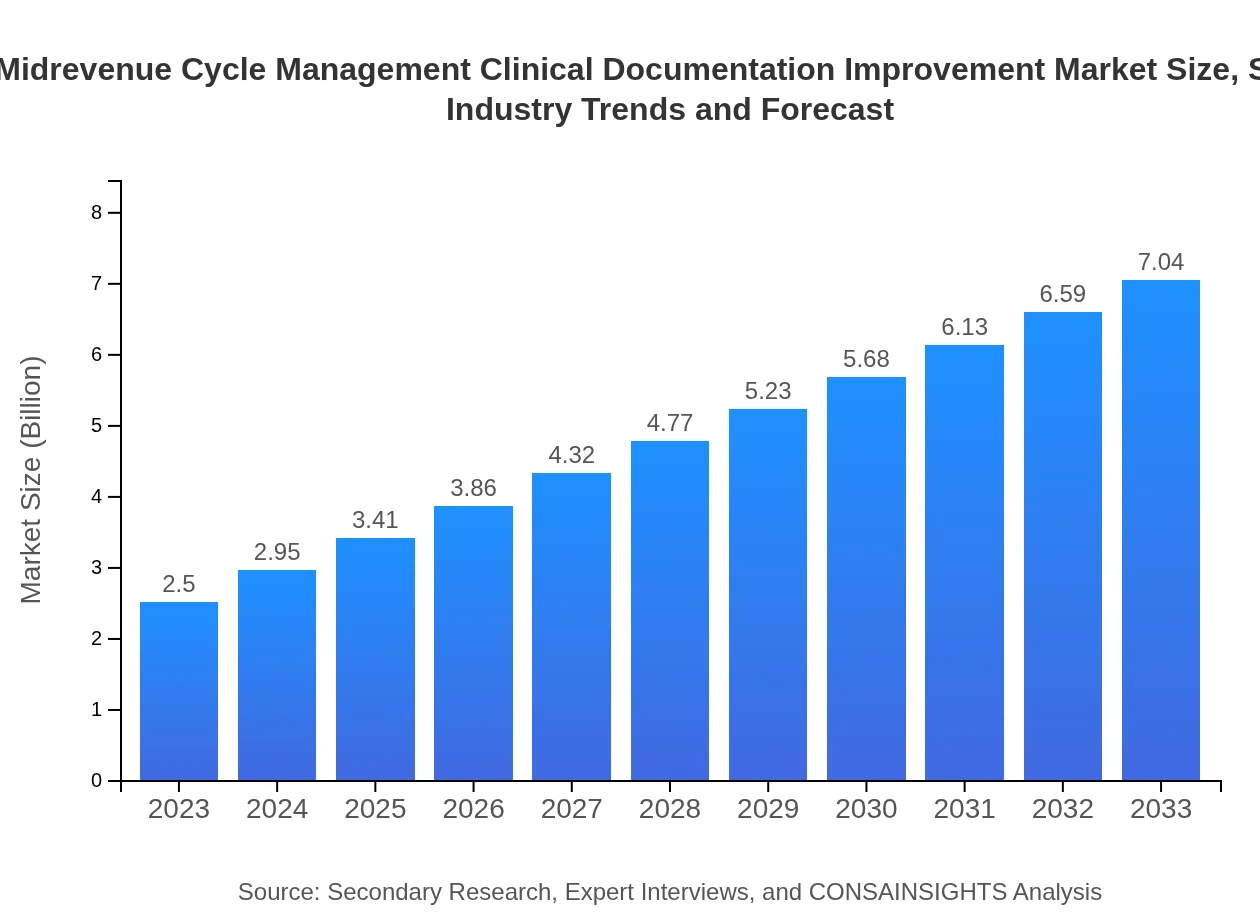
| Metric | Value |
|---|---|
| Study Period | 2023 - 2033 |
| 2023 Market Size | $2.50 Billion |
| CAGR (2023-2033) | 10.5% |
| 2033 Market Size | $7.04 Billion |
| Top Companies | Optum, R1 RCM, Cerner Corporation, MediSoft, 3M Health Information Systems |
| Last Modified Date | 31 January 2026 |
Midrevenue Cycle Management Clinical Documentation Improvement Market Overview
Customize Midrevenue Cycle Management Clinical Documentation Improvement Market Report market research report
- ✔ Get in-depth analysis of Midrevenue Cycle Management Clinical Documentation Improvement market size, growth, and forecasts.
- ✔ Understand Midrevenue Cycle Management Clinical Documentation Improvement's regional dynamics and industry-specific trends.
- ✔ Identify potential applications, end-user demand, and growth segments in Midrevenue Cycle Management Clinical Documentation Improvement
What is the Market Size & CAGR of Midrevenue Cycle Management Clinical Documentation Improvement market in 2023?
Midrevenue Cycle Management Clinical Documentation Improvement Industry Analysis
Midrevenue Cycle Management Clinical Documentation Improvement Market Segmentation and Scope
Tell us your focus area and get a customized research report.
Midrevenue Cycle Management Clinical Documentation Improvement Market Analysis Report by Region
Europe Midrevenue Cycle Management Clinical Documentation Improvement Market Report:
Europe’s MRCM CDI market is anticipated to grow from $0.75 billion in 2023 to $2.11 billion by 2033. The increase is attributed to stringent regulations aimed at improving healthcare documentation and a push towards adopting digital health solutions across the region.Asia Pacific Midrevenue Cycle Management Clinical Documentation Improvement Market Report:
In 2023, the MRCM CDI market in the Asia Pacific region is valued at approximately $0.46 billion, with projections to grow to $1.30 billion by 2033. The growth is fueled by increasing health IT adoption and government initiatives promoting electronic medical records (EMR). Countries like Japan and Australia are leading the shift towards advanced healthcare systems.North America Midrevenue Cycle Management Clinical Documentation Improvement Market Report:
In North America, the MRCM CDI market is projected at $0.93 billion for 2023, growing to $2.62 billion by 2033. The region dominates the market due to strong healthcare infrastructure, increasing demand for compliance with regulations, and a focus on optimizing reimbursement processes.South America Midrevenue Cycle Management Clinical Documentation Improvement Market Report:
The South American market stands at $0.23 billion in 2023, expected to reach $0.64 billion by 2033. Factors driving this growth include rising healthcare expenditures and a growing focus on improving health service delivery, although challenges such as regulatory hurdles persist.Middle East & Africa Midrevenue Cycle Management Clinical Documentation Improvement Market Report:
The Middle East and Africa market is relatively smaller, valued at $0.13 billion in 2023 with expectations to grow to $0.38 billion by 2033. The growth in this region will largely depend on increasing investments in healthcare infrastructure and enhanced regulatory frameworks.Tell us your focus area and get a customized research report.
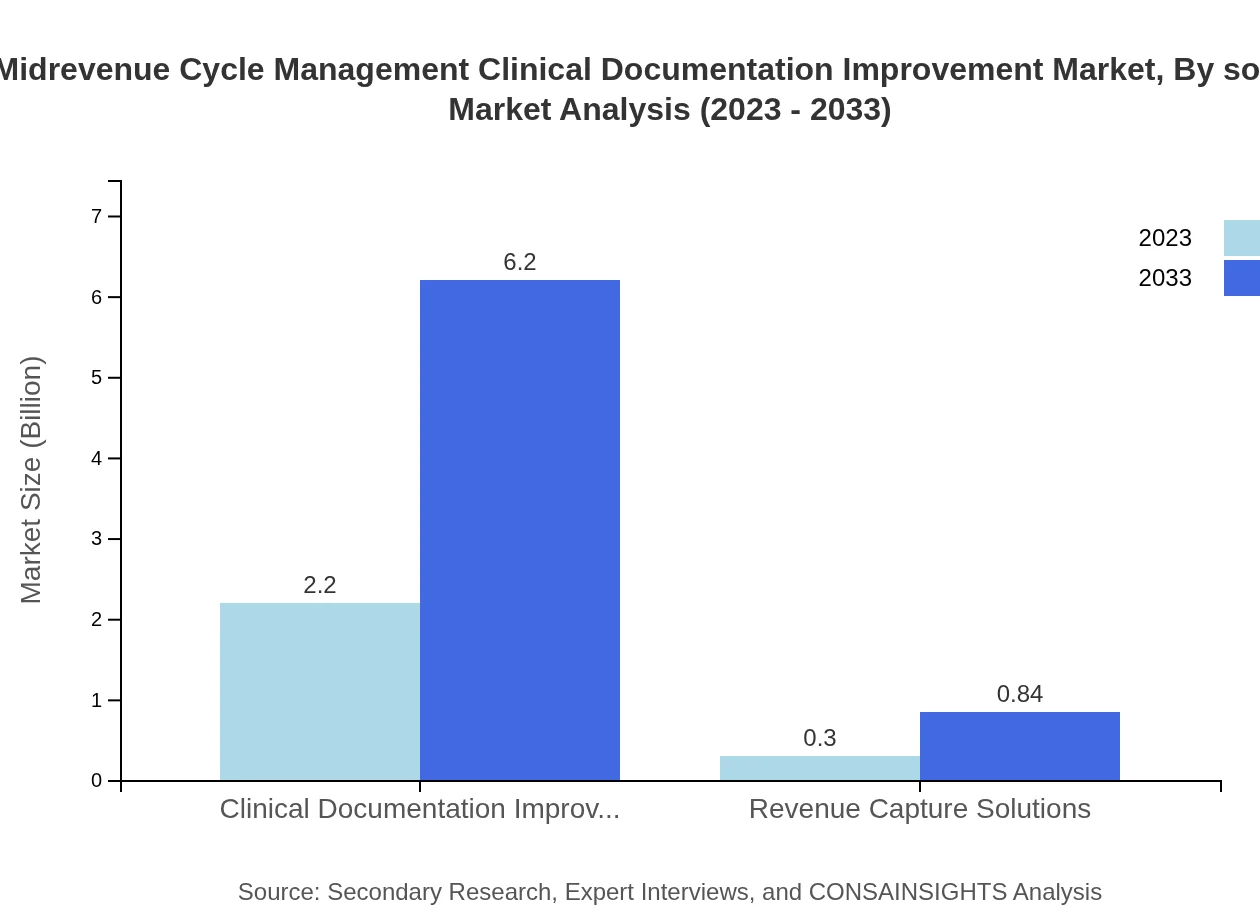
Midrevenue Cycle Management Clinical Documentation Improvement Market Analysis By Solution
In this segment, Clinical Documentation Improvement solutions dominate the market, accounting for $2.20 billion in 2023, increasing to $6.20 billion by 2033. Revenue Capture Solutions and consulting services also account for significant shares, reflecting a move toward integrated solutions in healthcare.
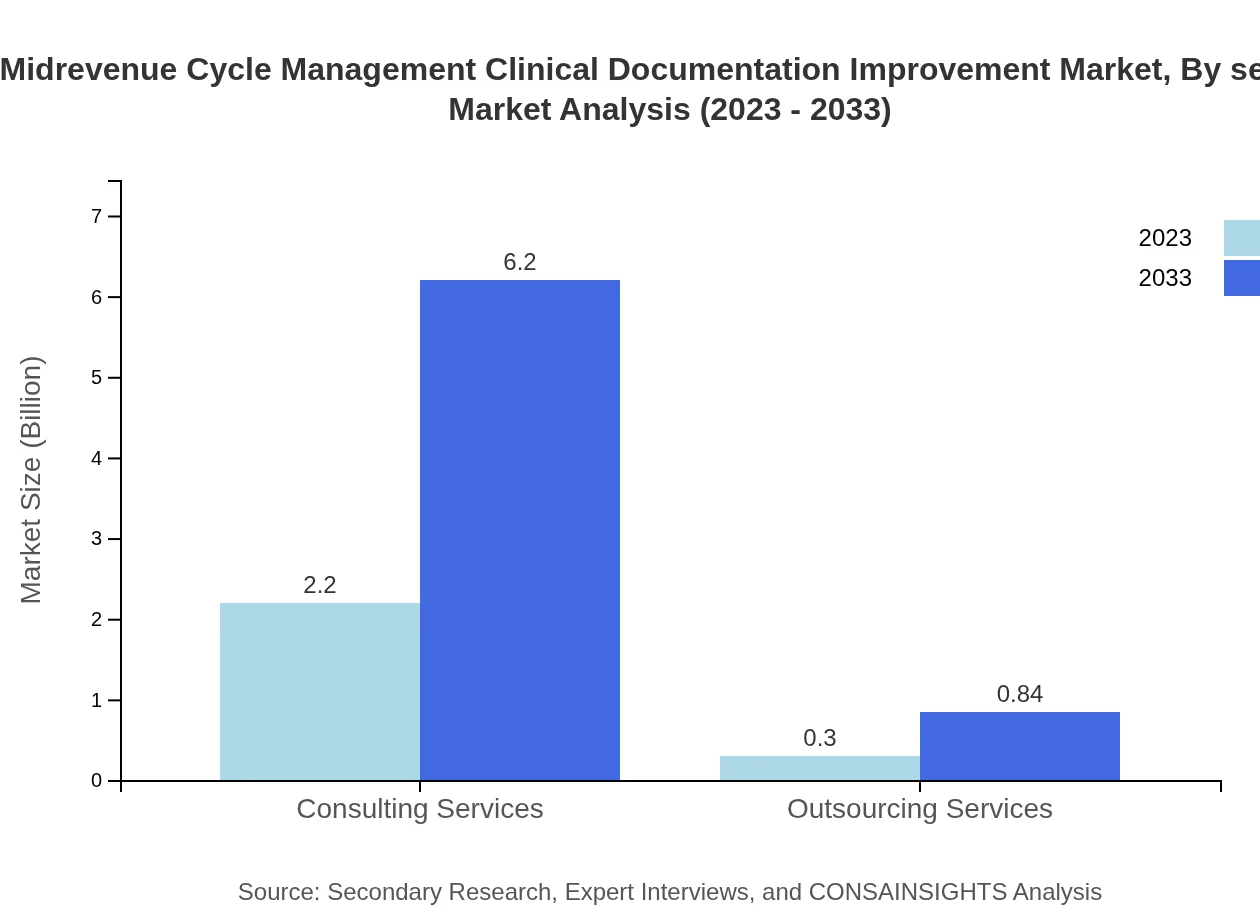
Midrevenue Cycle Management Clinical Documentation Improvement Market Analysis By Service
Consulting services are the leading segment, with a market size of $2.20 billion in 2023, projected to grow significantly over the next decade. Outsourcing services, although smaller, show a trend toward increased adoption as organizations look to cut costs and enhance operational efficiency.
Midrevenue Cycle Management Clinical Documentation Improvement Market Analysis By Deployment Type
The Cloud-based Solutions segment leads with an estimated market size of $2.20 billion in 2023, expected to grow to $6.20 billion by 2033, underscoring the trend towards digital transformation. On-premises solutions continue to serve specific operational needs but face declining demand.
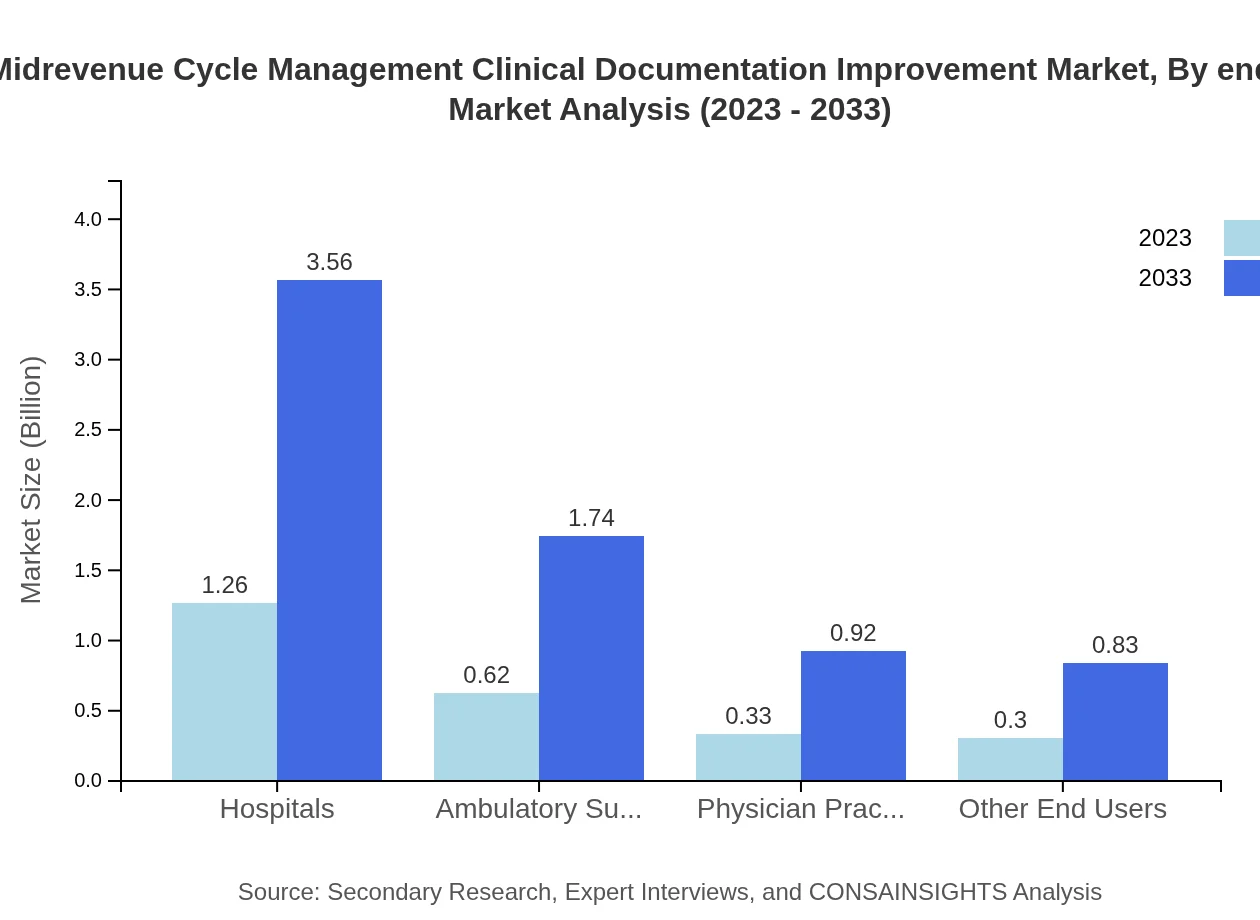
Midrevenue Cycle Management Clinical Documentation Improvement Market Analysis By End User
Hospitals represent the largest end-user segment, with a projected growth from $1.26 billion in 2023 to $3.56 billion by 2033, driven by the increasing need for compliant documentation and payment accuracy. Ambulatory Surgical Centers and physician practices are also pivotal players in this market landscape.
Midrevenue Cycle Management Clinical Documentation Improvement Market Trends and Future Forecast
Tell us your focus area and get a customized research report.
Global Market Leaders and Top Companies in Midrevenue Cycle Management Clinical Documentation Improvement Industry
Optum:
A leader in health services that provides software-driven solutions to improve clinical documentation and streamline revenue cycles for healthcare providers.R1 RCM:
Specializes in revenue cycle management and offers technology-enabled service solutions that enhance clinical documentation processes and operational efficiencies.Cerner Corporation:
Provides health information technology solutions and services, focusing on integrating clinical and revenue cycle management for enhanced documentation and reimbursement.MediSoft:
Develops comprehensive health IT solutions with a strong focus on clinical documentation improvement and revenue cycle optimization.3M Health Information Systems:
Offers innovative technology and solutions in clinical documentation improvement, focusing on maximizing revenue integrity and compliance.We're grateful to work with incredible clients.









FAQs
What is the market size of midrevenue Cycle Management Clinical Documentation Improvement?
The midrevenue cycle management clinical documentation improvement market is valued at approximately $2.5 billion in 2023, with a projected CAGR of 10.5%, indicating robust growth potential leading into 2033.
Who are the key market players or companies in this midrevenue Cycle Management Clinical Documentation Improvement industry?
The industry features key players focused on enhancing clinical documentation, including major healthcare consulting firms and technology solutions providers that specialize in revenue cycle management and clinical data analysis.
What are the primary factors driving the growth in the midrevenue Cycle Management Clinical Documentation Improvement industry?
Key growth drivers include increasing healthcare expenditures, the push for documentation accuracy, regulatory compliance demands, and technological advancements in healthcare analytics and management solutions.
Which region is the fastest Growing in the midrevenue Cycle Management Clinical Documentation Improvement?
The Asia Pacific region is the fastest-growing area, with the market anticipated to grow from $0.46 billion in 2023 to $1.30 billion by 2033, reflecting strong demand for healthcare improvements.
Does ConsaInsights provide customized market report data for the midrevenue Cycle Management Clinical Documentation Improvement industry?
Yes, ConsaInsights offers tailored market report data, ensuring customized insights that meet specific client needs and facilitate strategic decision-making within the midrevenue cycle management landscape.
What deliverables can I expect from this midrevenue Cycle Management Clinical Documentation Improvement market research project?
Deliverables typically include detailed market analysis reports, segmented data insights, trend forecasts, competitive landscapes, and recommendations tailored for strategic planning.
What are the market trends of midrevenue Cycle Management Clinical Documentation Improvement?
Current trends include a shift towards cloud-based solutions, increasing adoption of data analytics, and a growing focus on improving patient outcomes through enhanced documentation practices.