Referral Management Market Report
Published Date: 31 January 2026 | Report Code: referral-management
Referral Management Market Size, Share, Industry Trends and Forecast to 2033
This market report delves into the Referral Management industry, highlighting market size, growth forecasts, segmentation, and trends from 2023 to 2033. It offers valuable data-driven insights for stakeholders seeking to understand the future landscape of the market.
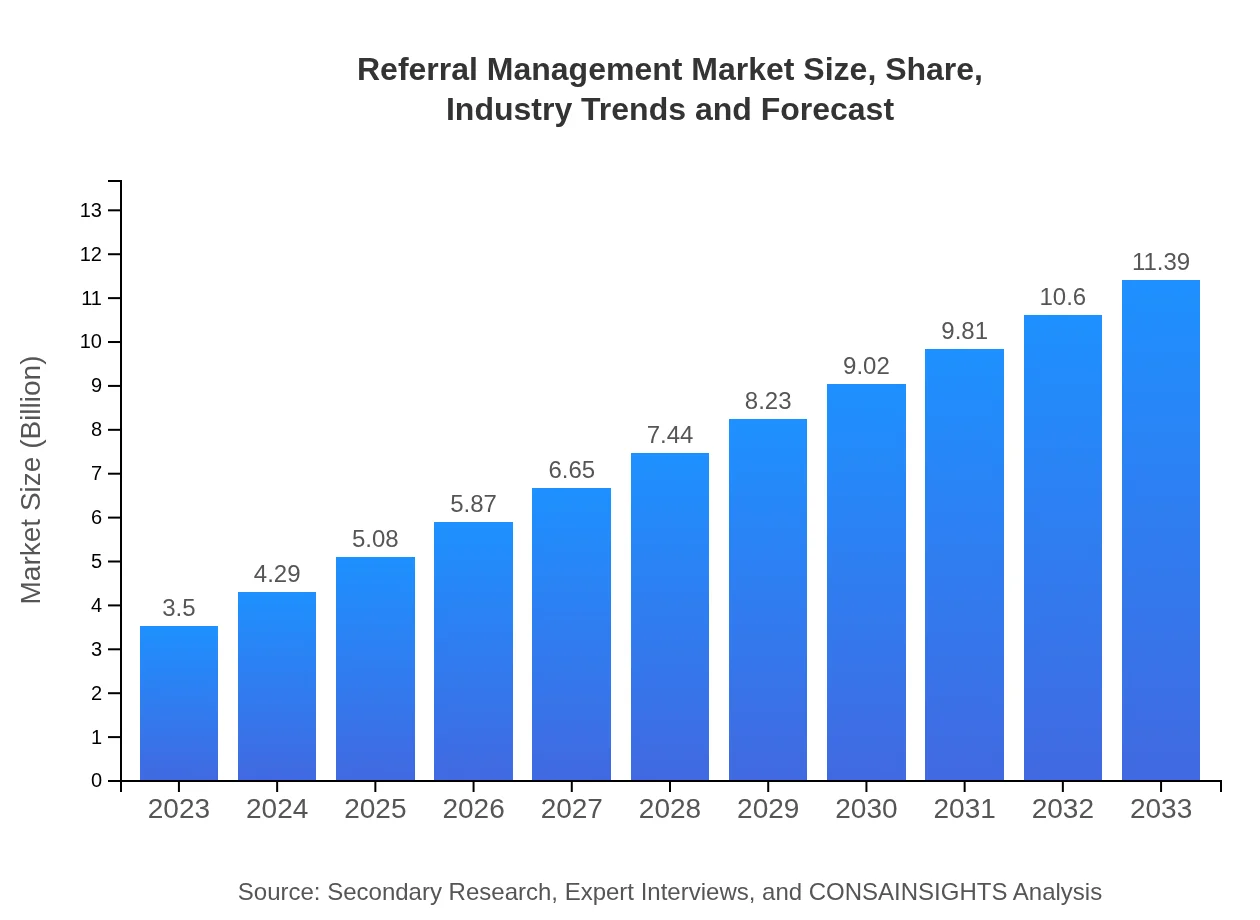
| Metric | Value |
|---|---|
| Study Period | 2023 - 2033 |
| 2023 Market Size | $3.50 Billion |
| CAGR (2023-2033) | 12% |
| 2033 Market Size | $11.39 Billion |
| Top Companies | Epic Systems Corporation, Cerner Corporation, Allscripts Healthcare Solutions, Meditech, Athenahealth |
| Last Modified Date | 31 January 2026 |
Referral Management Market Overview
Customize Referral Management Market Report market research report
- ✔ Get in-depth analysis of Referral Management market size, growth, and forecasts.
- ✔ Understand Referral Management's regional dynamics and industry-specific trends.
- ✔ Identify potential applications, end-user demand, and growth segments in Referral Management
What is the Market Size & CAGR of Referral Management market in 2023?
Referral Management Industry Analysis
Referral Management Market Segmentation and Scope
Tell us your focus area and get a customized research report.
Referral Management Market Analysis Report by Region
Europe Referral Management Market Report:
In 2023, the European Referral Management market stands at $1.24 billion, anticipated to grow to $4.02 billion by 2033. Factors such as an aging population, regulatory support for centralized health data systems, and the increasing integration of digital solutions in healthcare drive significant growth across countries like Germany, France, and the UK.Asia Pacific Referral Management Market Report:
In 2023, the Referral Management market in the Asia Pacific region is valued at approximately $0.56 billion and is forecasted to grow to $1.84 billion by 2033. The growth is driven by increasing healthcare expenditures, a rising number of healthcare facilities, and greater adoption of IT solutions to improve patient management. Countries like India and China are leading this growth through their expanding healthcare infrastructure and governmental support for digital health initiatives.North America Referral Management Market Report:
North America boasts a substantial market size of approximately $1.21 billion in 2023, expected to surge to $3.92 billion by 2033. This region leads the market due to advanced healthcare systems, significant investments in healthcare IT solutions, and a robust focus on improving patient outcomes. The U.S. is a major contributor, driven by the high prevalence of chronic diseases requiring effective referral processes.South America Referral Management Market Report:
The South American market, valued at $0.29 billion in 2023, is projected to reach $0.93 billion by 2033. Growth is propelled by an increased emphasis on healthcare accessibility, improvements in primary care networks, and governmental policies aimed at strengthening healthcare delivery systems. Brazil and Argentina are particularly noteworthy for their investments in health technologies.Middle East & Africa Referral Management Market Report:
The Middle East and Africa market is relatively smaller, valued at $0.21 billion in 2023 and expected to grow to $0.68 billion by 2033. The increasing investment in healthcare infrastructure and a growing awareness of the importance of integrated care models contribute to market growth. The region is gradually adopting digital solutions to address healthcare challenges.Tell us your focus area and get a customized research report.
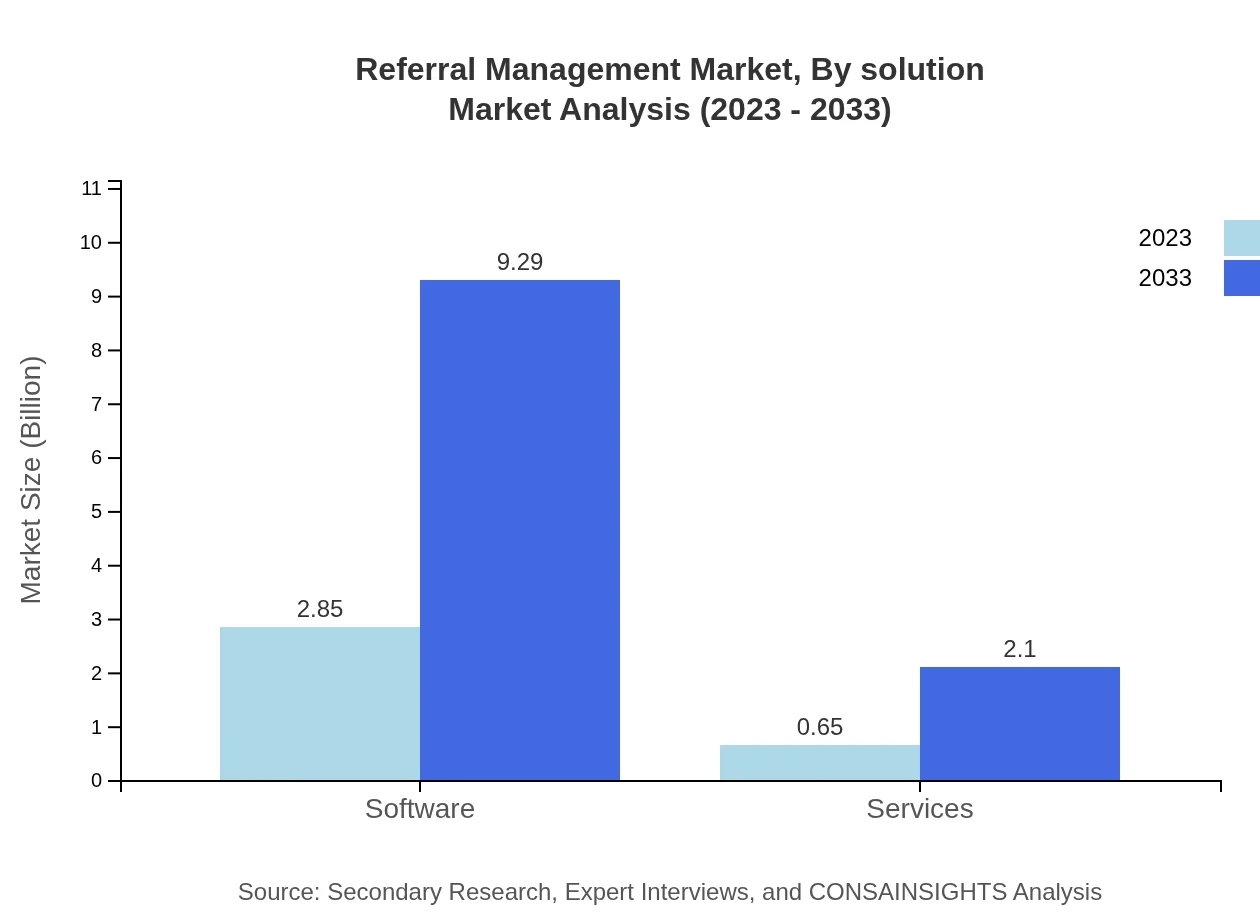
Referral Management Market Analysis By Solution
In 2023, the software segment dominates the Referral Management market, accounting for a market size of approximately $2.85 billion, which is expected to grow to $9.29 billion by 2033. Cloud-based solutions constitute a significant part of this segment, representing 81.55% market share in 2023. The services segment, providing essential support and maintenance, is projected to grow from $0.65 billion in 2023 to $2.10 billion by 2033.
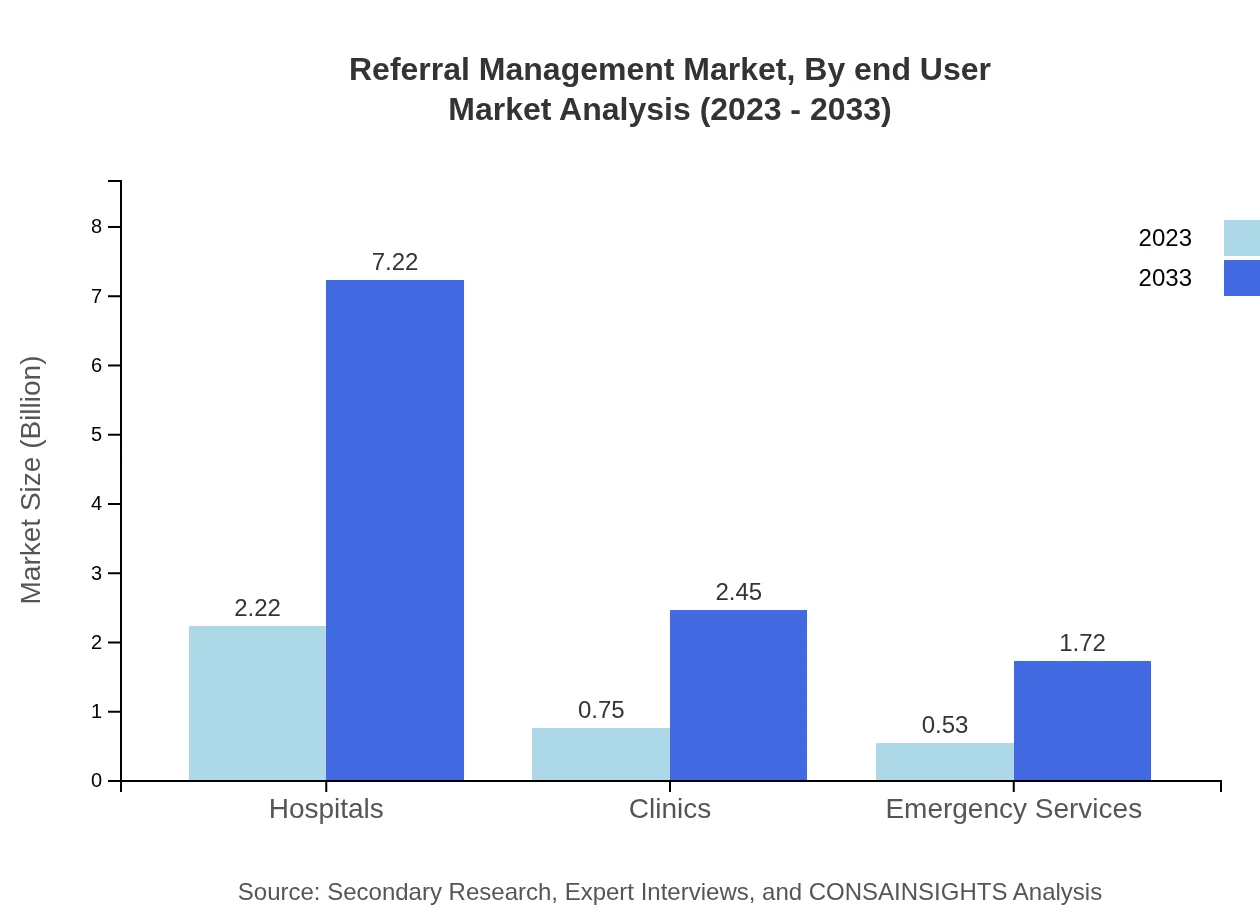
Referral Management Market Analysis By End User
Hospitals lead the Referral Management market with a substantial share of 63.38% in 2023, anticipated to remain consistent through 2033, growing from $2.22 billion to $7.22 billion. Clinics represent 21.55% of the market share, increasing from $0.75 billion in 2023 to $2.45 billion by 2033, while emergency services hold a 15.07% share, with growth from $0.53 billion to $1.72 billion over the same period.
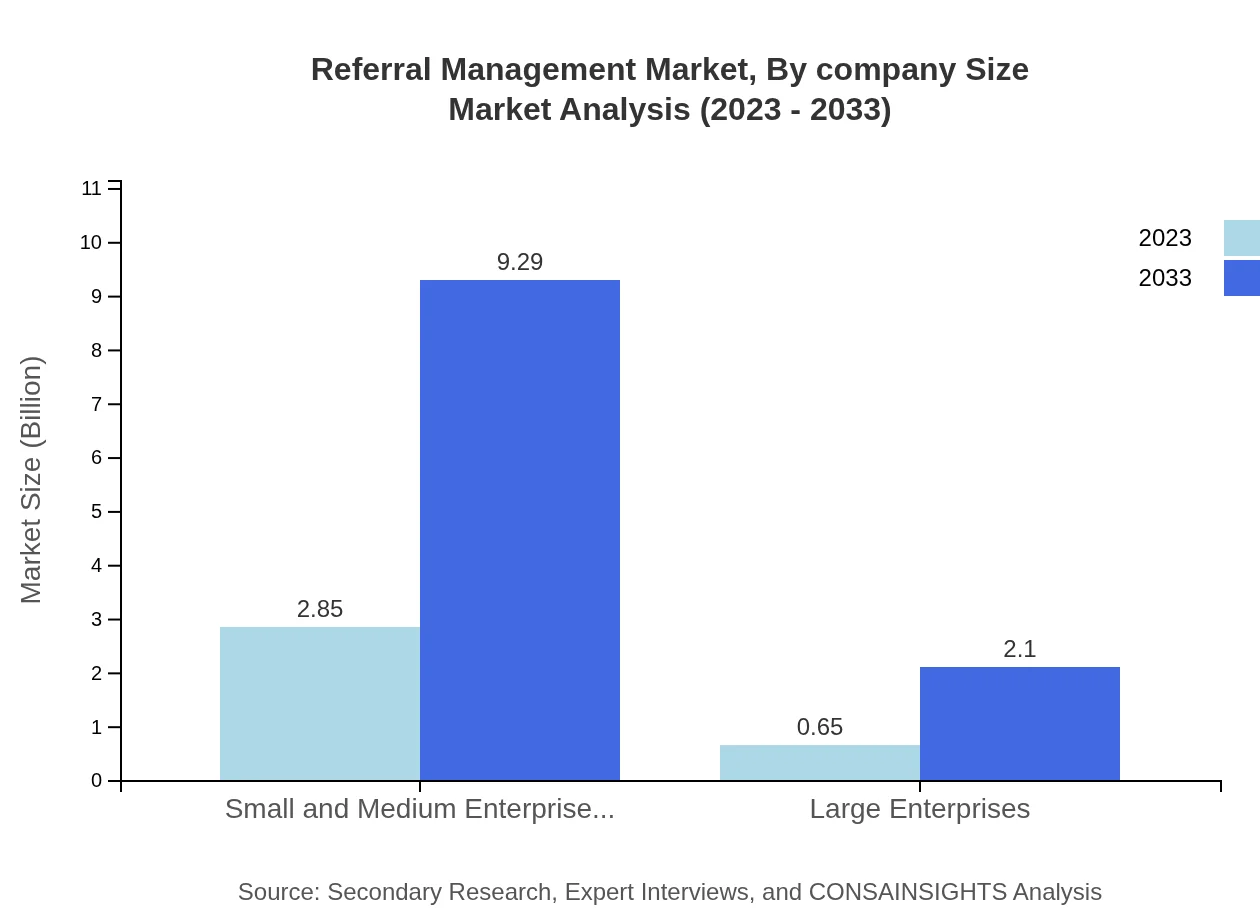
Referral Management Market Analysis By Company Size
Small and medium enterprises (SMEs) represent the majority of the Referral Management market, comprising 81.55% market share and growing from $2.85 billion in 2023 to $9.29 billion by 2033. Large enterprises, while smaller in share at 18.45%, are also expected to see growth from $0.65 billion to $2.10 billion, reflecting their increasing investment in comprehensive referral management solutions.
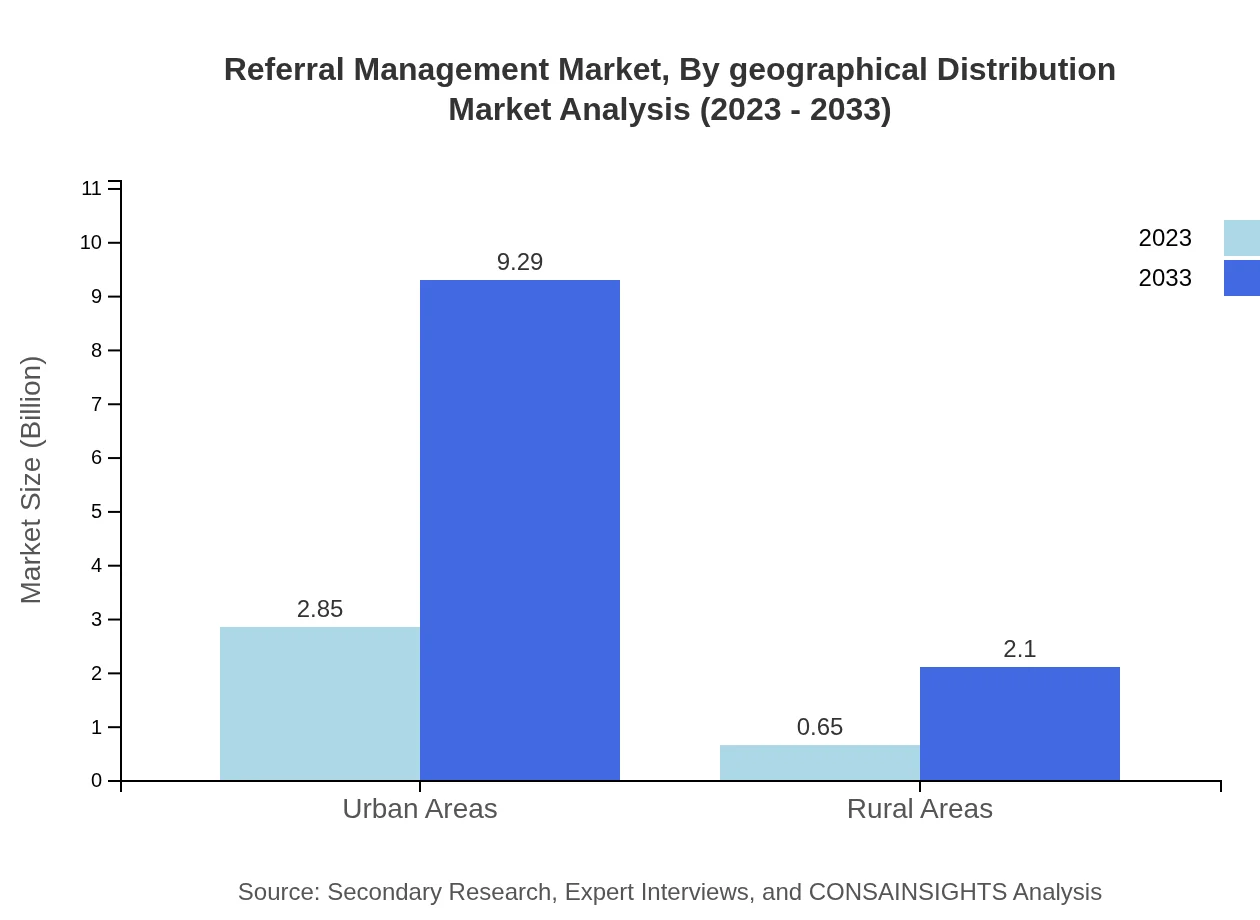
Referral Management Market Analysis By Geographical Distribution
The geographical distribution of the Referral Management market reveals significant growth across major regions. North America holds a large market share, driven by technological advancements and healthcare integration. Europe follows closely, with substantial investments in health tech, while the Asia Pacific region shows high growth potential due to rising urbanization and healthcare demands. South America and the Middle East/Africa represent emerging markets, with improving healthcare infrastructure boosting adoption rates.
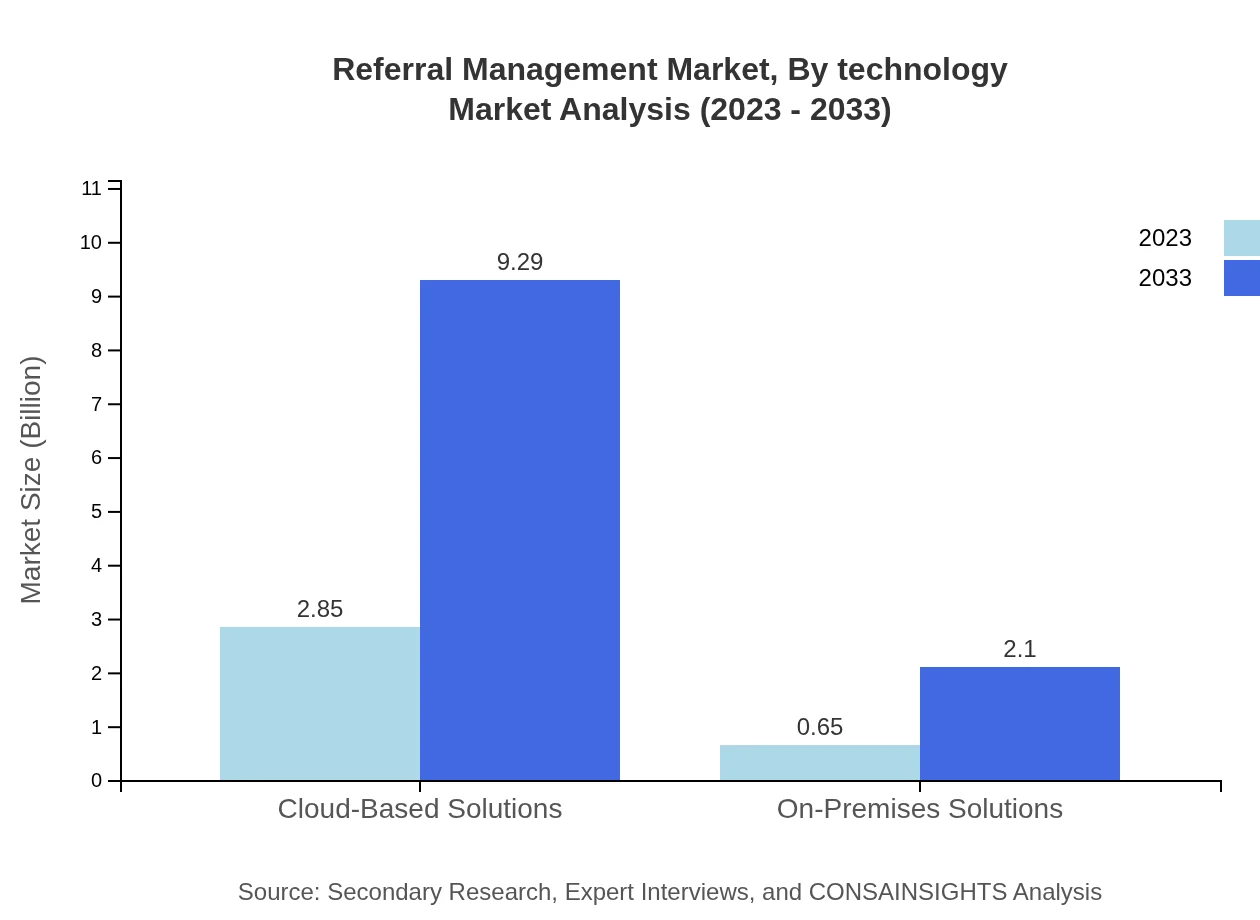
Referral Management Market Analysis By Technology
Innovations in technology, such as artificial intelligence, predictive analytics, and telehealth solutions, are transforming the Referral Management landscape. Cloud-based systems enhance scalability and data sharing capabilities, while AI-driven insights improve referral processes and patient tracking. These technological advancements are vital as healthcare evolves towards more integrated, patient-centric models, positioning tech-savvy organizations as leaders in the market.
Referral Management Market Trends and Future Forecast
Tell us your focus area and get a customized research report.
Global Market Leaders and Top Companies in Referral Management Industry
Epic Systems Corporation:
A leading health informatics company, Epic provides software solutions that enhance patient management and facilitate seamless referral workflows in healthcare organizations.Cerner Corporation:
Cerner's suite of healthcare solutions includes comprehensive referral management software, empowering hospitals and clinics to improve care coordination capabilities.Allscripts Healthcare Solutions:
Allscripts offers flexible and scalable health IT solutions, focusing on enhancing referral processes with integrated data sharing functionalities.Meditech:
Meditech specializes in health IT solutions including EMR and referral management systems, supporting healthcare providers in optimizing patient care pathways.Athenahealth:
Athenahealth provides cloud-based solutions for healthcare organizations, streamlining referral processes and contributing to enhanced patient engagement and overall care quality.We're grateful to work with incredible clients.









FAQs
What is the market size of referral Management?
The referral management market is valued at $3.5 billion in 2023, with a projected CAGR of 12% leading to substantial growth by 2033.
What are the key market players or companies in this report name industry?
Key players in the referral management industry include major healthcare IT providers, telecommunications companies, and innovative startups focusing on healthcare solutions.
What are the primary factors driving the growth in the referral management industry?
Growth is primarily driven by the increasing need for coordinated healthcare services, advancements in digital health technology, and the emphasis on patient-centered care delivery.
Which region is the fastest Growing in the report name?
The fastest-growing region in the referral management market is Europe, projected to grow from $1.24 billion in 2023 to $4.02 billion by 2033.
Does ConsaInsights provide customized market report data for the report name industry?
Yes, ConsaInsights offers customized market report data tailored to specific needs and inquiries in the referral management sector, ensuring relevant insights.
What deliverables can I expect from this report name market research project?
Expect comprehensive insights including market analysis, competitor reviews, segmentation data, and strategic recommendations tailored for the referral management market.
What are the market trends of referral management?
Key trends include the rising adoption of cloud-based solutions, the integration of AI in healthcare, and the focus on improving patient experience through effective referral systems.